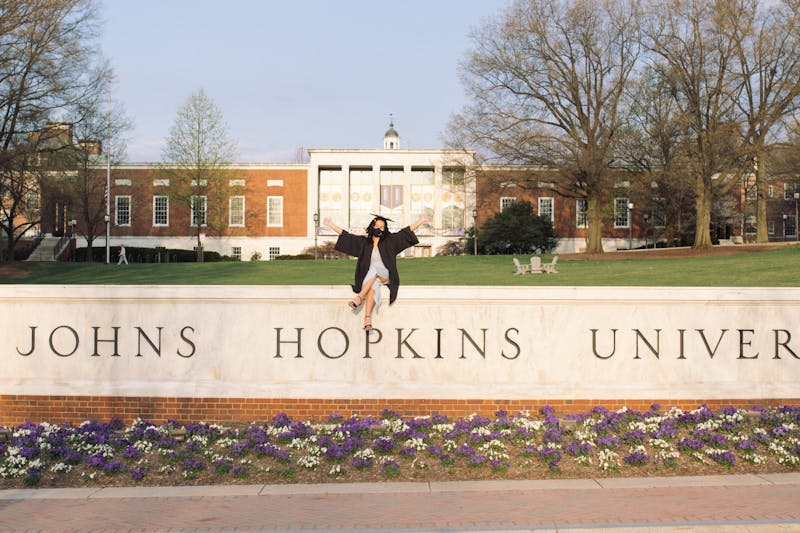
COURTESY OF AMANI NELSON
While she appreciates her time at Hopkins, Nelson is concerned that public health coursework fails to meaningfully address anti-Blackness in health care.
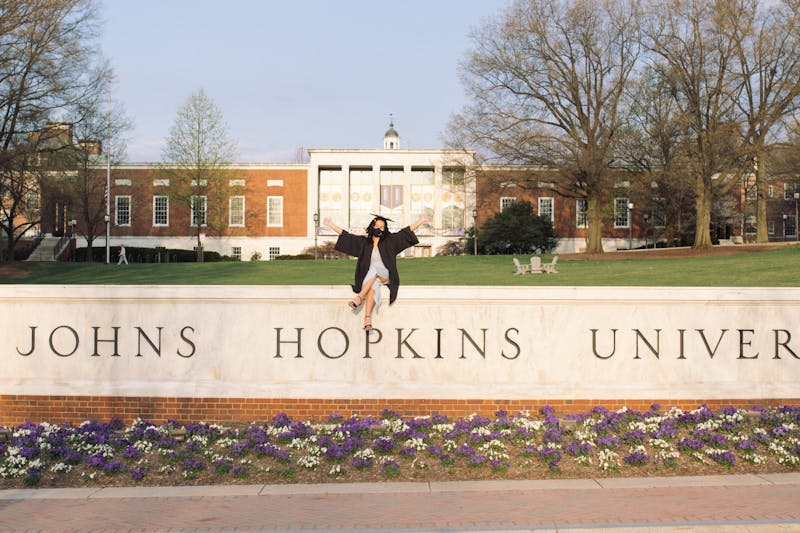
COURTESY OF AMANI NELSON
While she appreciates her time at Hopkins, Nelson is concerned that public health coursework fails to meaningfully address anti-Blackness in health care.
Editor’s Note: The original title of this piece failed to accurately reflect the author’s sentiments and has been updated accordingly.
When I was a freshman at Hopkins, I used to wander through different dorms at night looking for new people. Before COVID-19, this was how I made a lot of friends: having meaningful late-night conversations over Insomnia cookies or fruit snacks. One evening, I met a few fellow freshman Public Health majors. We started discussing what areas of study we were interested in and I mentioned maternal and child health.
When asked what drew me to this subject, I said that I mainly wanted to protect Black women, especially after what happened to Serena Williams. They gave me a puzzled look and asked what I was talking about. While I was a little surprised they were unaware of the story, I briefly recounted tennis legend Serena Williams’ terrifying experience giving birth to her daughter Olympia. Because her doctors ignored her reports of severe pain, she nearly lost her life to blood clotting.
My new friends were understandably enraged when I told them this story, and even more so when I explained that this sort of thing happens all the time. I also added that, while what happened to her was awful, she is one of the most inspiring people and went on to continue dominating the tennis world just ten months after giving birth.
Looking back on my four years at Hopkins, this interaction still stands out to me. I was glad to have the chance to educate some future doctors on the kind of medical racism that is often ignored. However, I still feel a sense of worry over what these students are missing out on. Not only an ugly truth about the medical field, but also the truth about Black people and our experiences. Not all good, but certainly not all bad, much like Serena Williams’ birth story.
In my own house, being Black was synonymous with excellence. Excellence in athletics, academics and any challenge life would throw my way. It meant having strong family, religious and social ties. I had role models everywhere, from Simone Biles to my own father. Still, I saw problems too. I saw friends and family abused or ignored by medical professionals. I couldn’t understand why so many people I knew had fibroid cancer, childbirth complications or horrendous experiences with the health-care system. I wanted to learn how to change these problems, and what better way to do so than to study public health at Hopkins?
I learned a lot in my coursework at Homewood and the School of Public Health. I learned how to read and write scientific literature and to conduct research. I even got the chance to volunteer at different community organizations. But the attitudes towards Blackness and Black people were very different from what I knew.
For the past four years I have sat in lecture halls being told that being Black is a “risk factor” for so many deadly diseases and conditions when, in reality, race is never a risk factor. Racism is. Even when the appropriate language was used, I was always taught that being Black and being poor were synonymous, or that being Black meant being at risk for diabetes, HIV and poor health care. Conversely, I was taught that being white was synonymous with wealth, regular doctor’s visits and “better” health behaviors.
Not once did a professor mention how African Americans have one of the lowest suicide rates despite the current mental health crisis we are witnessing. I was never taught about the high college education rates for Black women. Many classes discussed drug use in the Black community as if it were rampant when, in reality, Black undergraduates have lower rates of drug use than their white peers.
At a university where I was encouraged to ask questions and research, no one was able to explain the social determinants of Black excellence, only Black suffering. And even the explanations of Black suffering seemed to miss the fact that doctors and other health professionals, the very people so many of my peers were striving to be, were the direct cause of so much neglect, abuse and death.
I have been able to fill these gaps in my education through firsthand and secondhand experiences, but I didn’t stop there. I read books, papers and the current literature on the reality of African American health. I would encourage all my fellow students to do the same.
I don’t write this to tear down or diminish the good work being done by the faculty at Hopkins and the School of Public Health. I have learned invaluable information from these schools and I look forward to applying in my future career. However, educating the future doctors of America means being honest about anti-Blackness in the health-care system beyond just a single lecture on the Tuskegee Study. It also means putting as much effort into studying Black achievement as you do Black adversity.