Epilepsy is a disorder characterized by disturbances in neuronal activity resulting in seizures. One in 26 people will develop epilepsy during their lifetime.
Epilepsy diagnosis is an imperfect science. Approximately 30% of patients are misdiagnosed after their first visit. Consequences of these misdiagnoses can be severe: Untreated epilepsy increases seizure frequency and can be fatal, but at the same time, false positive results are equally dangerous. Patients who receive false diagnoses of epilepsy can face unnecessary discomfort and receive unnecessary treatments with significant side effects.
To combat misdiagnosis, a team of researchers at Hopkins led by Dr. Sridevi Sarma — professor in the Department of Biomedical Engineering and vice dean for graduate education at the Whiting School of Engineering — developed EpiScalp: a machine-learning-based tool that analyzes routine scalp electroencephalograms (EEGs). EpiScalp has demonstrated profound potential in identifying epilepsy for many patients, especially for those with EEGs that initially appear normal to the human eye.
The sensitivity of a routine EEG for epilepsy diagnosis is fairly low, ranging from 25%–55%. Traditional diagnosis relies on the identification of epileptiform discharges, the distinctive electrical patterns in the brain that are indicators for epilepsy. However, these discharges are often sporadic and may not be present during a routine EEG recording.
As a result, many patients have completely normal EEGs despite having epilepsy. In an interview with The News-Letter, Dr. Khalil Husari — a neurologist at the Hopkins Hospital and assistant professor of Neurology — further explained some of the other problems with current epilepsy diagnosis.
“The diagnosis of epilepsy is predominantly a clinical diagnosis and depends on what the patient tells you. In some patients, it will be a straight diagnosis...however in other patients, the diagnosis can be not as straightforward, for example, if there’s no collateral information,” he said. “This is particularly common because the patients are typically amnestic, they lose consciousness and they can’t remember exactly what happened...In these cases, ancillary studies help neurologists and the clinician make the diagnosis...but if the EEG is normal, that will not add much.”
EpiScalp uses a machine learning model trained on retrospective data from 198 patients from the Epilepsy Monitoring Unit (EMU). By analyzing EEG connectivity patterns, the model assigns a risk score between zero and one, indicating the likelihood of epilepsy. In a clinical study, EpiScalp significantly reduced the misdiagnosis rate from 54% to 17%.
Developing EpiScalp required overcoming several computational challenges. According to Sarma, perhaps the most daunting challenge was determining whether the brain contained hidden markers of epilepsy that conventional analysis methods overlooked, which could hopefully lead to the discovery of the biological basis behind the tool.
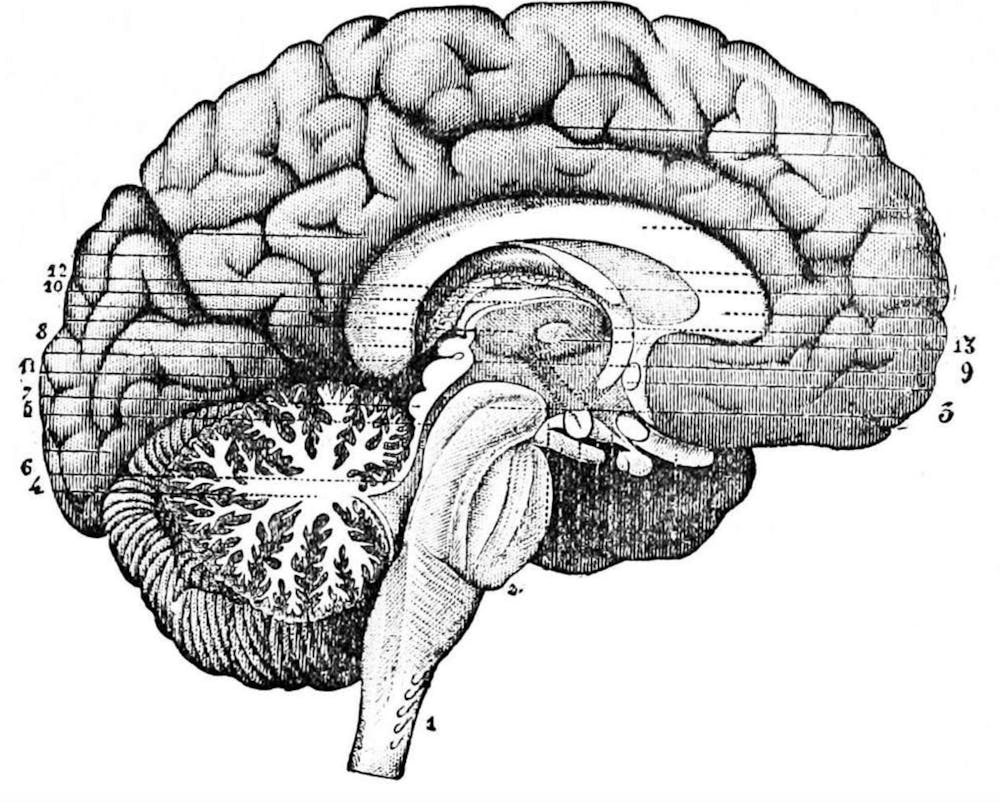
The answer, they found, lay in a larger-scale network analysis to see how epilepsy impacted these interconnections and relationships between neurons. Rather than searching for epileptiform discharges in EEGs, EpiScalp examines how brain regions interact with one another.
The underlying hypothesis for this mechanism is that in patients with epilepsy, the brain exhibits altered connectivity patterns even when a seizure isn’t occurring.
Researchers hypothesized the existence of an “epileptogenic zone” in the brain of epileptic patients that was responsible for seizure activity. This area was predicted to be inhibited by another brain region when the patient was not seizing.
Sarma elaborated on the biological basis for the tool in an interview with The News-Letter.
“There’s an area in the brain, even if it’s generalized, it starts somewhere...but it’s an epileptogenic region...so that exists in the brain all the time...when you’re not seizing, we believe that it’s because other areas of the brain are inhibiting,” she explained.
Researchers searched for the group of “nodes” responsible for inhibiting the epileptogenic zone which would only exist in epilepsy patients, thus identifying these as targets for their software to use when diagnosing epilepsy.
EpiScalp was designed with clinical usability in mind. The system can be integrated into existing EEG software with minimal disruption to current workflows.
“Once an EEG is captured, EpiScalp runs as a software application that processes the data and generates a risk score in real time,” Sarma elaborated.
The tool has its own graphical user interface, making it easy for clinicians to interpret results alongside traditional EEG readings.
Looking ahead, the researchers plan to conduct validation studies to reproduce EpiScalp’s success in larger patient populations. They hope to eventually integrate the software fully into a clinical setting.
EpiScalp represents a significant step forward in epilepsy diagnosis. By moving beyond conventional EEG analysis, this breakthrough software has the potential to reshape how clinicians detect and manage epilepsy, substantially improving patient outcomes.