As we continue to push through the spring semester, take a break and catch up with some of the latest scientific discoveries.
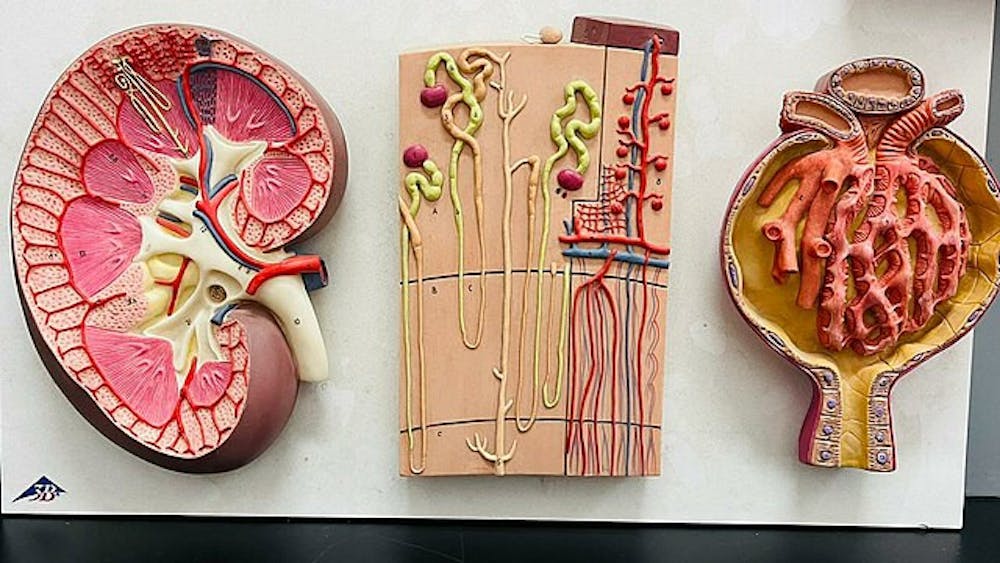
Massachusetts General Hospital transplants a pig kidney into a human
On Jan. 25, a patient with end-stage kidney disease, Tim Andrews, received a porcine kidney transplant at Massachusetts General Hospital. This procedure was the fourth time a genetically-edited porcine kidney was purposed for human use, and two more patients will undergo the same procedure as part of a clinical trial involving eGenesis, a pharmaceutical company.
The kidney was genetically edited 69 times using CRISPR-Cas9 to prevent the potential of an immune rejection, which occurs when the patient’s immune system recognizes the transplanted organ as foreign, by removing harmful pig genes and adding certain human genes. A transplant rejection can be categorized as either hyperacute, acute or chronic, distinguished by how long the body takes to reject the organ as well as the molecular mechanisms of the rejection. For patients that undergo allotransplantation —transplantation between individuals of the same species — patients take immunosuppressive medication such as calcineurin inhibitors and glucocorticoids to prevent rejection. To compensate for the differences that occur with xenotransplantation — the transplantation that occurs between different species —researchers utilize gene editing technology in addition to the patients taking immunosuppressants.
One of the many edits to the kidney included inactivating porcine endogenous retroviruses, which are present in all porcine genomes and can infect and replicate in humans as well.
Recent study advances characterization of the the unique genetics of Indigenous people in Greenland
A study recently published in Nature has analyzed the genomes of 5,996 people living in Greenland — around 14% of the territory's population at the time this study took place. Around 90% of Greenland’s population are Greenlandic Inuit, also known as Greenlanders, but there is a gap in knowledge regarding the genetic information of this group, partially due to the underrepresentation of indigenous populations in research.
An aspect of the study examined the population bottleneck that might have caused a different genetic distribution compared to other Indigenous populations. A minority of the study subjects’ genetic makeup was examined through whole-genome sequencing, averaged out over 35 times. The rest were studied by analyzing their single nucleotide polymorphisms (SNP), single-nucleotide variants in a DNA sequence, using SNP arrays. The prior dataset served as a reference to impute the rest of the missing SNP data of the latter group. This collection of genetic information can then be used to learn more about certain diseases and how they impact the Greenlandic Inuit population.
Pancreatic cancer detection by nanosensor assay
Around 70,000 people are diagnosed with pancreatic cancer each year and the disease is one of the most fatal types of cancer. Proteases — enzymes that catalyze the breakdown of proteins and are involved in digestion and other processes — can be studied as an indicators of cancer since increased protease activity contributes to the breakdown of the extracellular matrix and can facilitate tumor cell invasion and metastasis.
In a study published in Science Translational Medicine, a protease-activated nanosensor assay was developed to detect pancreatic cancer. The researchers of the study specified matrix metallopeptidase 2, an enzyme that plays a significant role in peptide cleavage and the degradation of the extracellular matrix, as an enzyme of interest. In this assay, a fluorescently labeled peptide sequence is linked to a magnetic iron oxide nanoparticle. When the matrix metallopeptidase 2 enzymes from a patient’s collected blood sample cleave the peptides, the fluorescent parts are released into the solution. The intact nanoparticles are then removed using their magnetic properties, leaving only the cleaved fluorescent fragments, which can be measured for quantification.
With this technology, which is relatively inexpensive and easy-to-access tool compared to current products, the researchers hope to increase the accuracy of pancreatic cancer diagnosis.