Dr. Won Jin Ho presented a talk as part of the Immunology Neighborhood Seminar on “Overcoming the tumor immune microenvironment — barriers to cancer immunotherapy” on Jan 21. Ho is a physician-scientist at the Sidney Kimmel Comprehensive Cancer Center and director of the Mass Cytometry Director at the Johns Hopkins School of Medicine.
Ho’s expertise centers on pancreatic and liver cancer immunology. He emphasizes that immunotherapy is a mainstay in cancer treatment.
“If you look at 2019 data, half of the patients diagnosed with cancer are eligible for some checkpoint immunotherapy. That’s really a pillar of cancer therapy at this moment,” he said.
However, most cancers are not as sensitive to provoke an immune response as physicians hope, and reductions in cancer burden (defined as a 30% reduction in tumor volume) is only observed in 20-30% of all cancers treated with more than two immunotherapy checkpoints. In essence, only about one-third of patients who received two or more types of immunotherapy treatments responded in a significant manner. Others were hindered by immunotherapy resistance–limited by cancer cells that develop resistance to immunotherapy checkpoint treatments.
Ho’s research team studies the immunogenic features of pancreatic ductal adenocarcinoma (PDAC). PDAC is the prototype for immune resistance, characterized by high mortality and metastasis rates as well as the “immunologically cold” characteristic of PDAC.
To address this, scientists have pioneered vaccines to help the immune system recognize and fight cancer cells. The first proof of concept of a cancer vaccine is with a GVAX, which uses genetically modified tumor cells to stimulate the immune system to attack cancer cells. In neoadjuvant studies, patients will receive the vaccine and then go on to surgery to resect the tumor. Researchers can then study the immune infiltration in the tumor tissue.
“We have phenological success with these agents. We can bring in immune cells, which is what we want,” Ho said. “But disease still recurs in most patients. So why is that?”
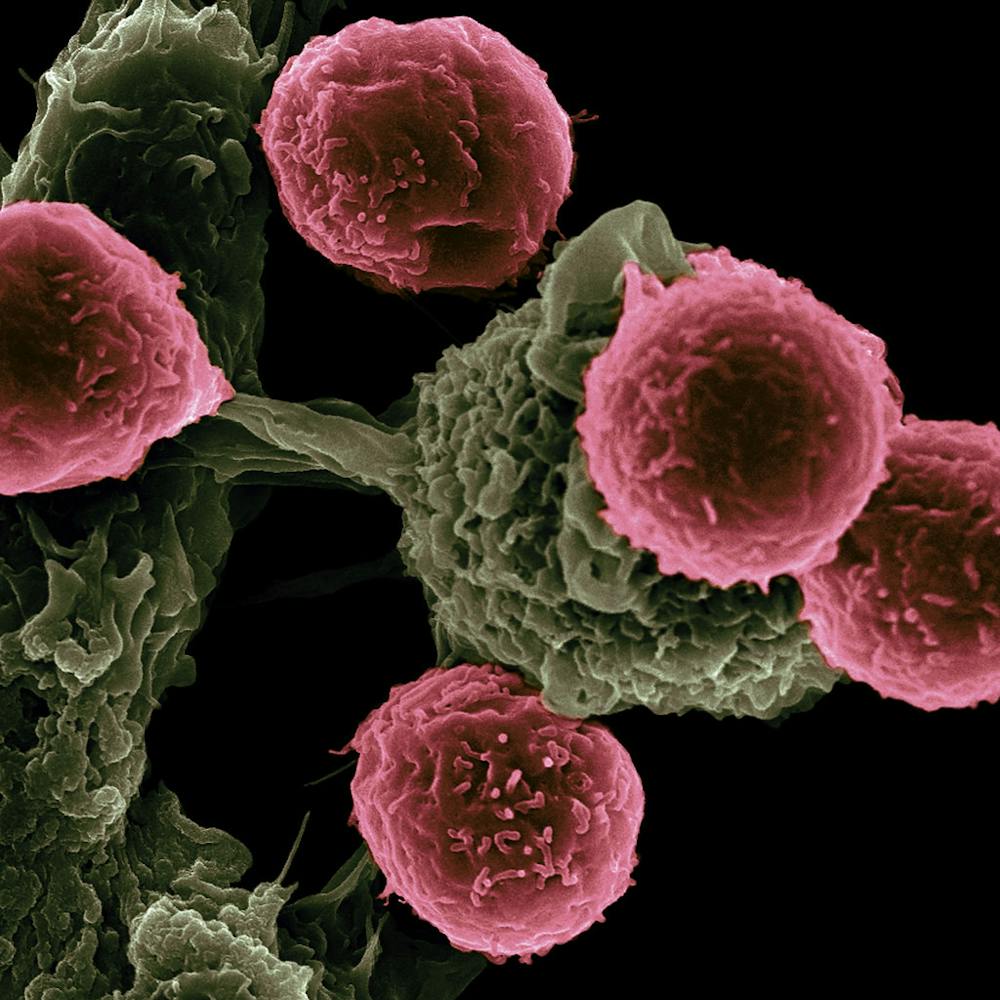
To answer this question, Ho focuses on the tumor microenvironment in PDAC, which consists of cancer fibroblasts, myeloid cell subtypes and T cell subtypes. Ho aims to discover what is preventing immune cells from entering the microenvironment and attacking cancer cells. At the Johns Hopkins Hospital, there are many clinical trials and specimens that allow for the bedside–bench–bedside approach to answer Ho’s question.
CXCL12 is a stromal fibroblast that is very rich in cancer cells, and the target of Ho’s lab. Fibroblasts are very prominent in pancreatic cancer.
CXCL12 can act as a glue for immune cells, anchoring them outside the tumor environment and preventing immune attacks, resulting in fewer anti-tumor functions. As such, blocking this pathway would increase immunotherapy (anti-PD1 therapy) efficacy. In a clinical trial for metastatic breast cancer patients, a team of researchers at Hopkins used a combined CXCL4 clinical inhibitor and anti-PD1 to assess response rate. Unfortunately, this trial yielded no response.
Ho then analyzed the data to find the reason for the non-response. His team was able to find CD34+ cells and more immune cells in circulation by CyTov. The treatment also mobilized myeloids evidenced by upregulation of other chemokine pathways. Looking at the tissue through serial biopsy, Ho’s team confirmed by H&E staining that the treatment decreased inflammation in the tumor tissue.
Through mass cytometry, his team also found an influx of immune cells in the microenvironment. Using cell segmentation and single-cell phenotyping algorithms, he was able to distinguish cell phenotypes and visualize the spatial distance between the networks of cell clusters.
“What’s interesting is that we have the different subtypes of macrophages, their proximity to T cells becomes much closer… But importantly, granulocytes don’t behave the same way… granulocytes actually have a greater distance to T cells,” he added.
From this data, Ho hypothesized that macrophages are responsible for immunosuppressive characteristics in PDAC. In mouse models, there was no clinical response, but there was an increased number of macrophages in the tumor microenvironment. When the macrophages in the tumor microenvironment were targeted, this yielded higher anti-tumor effects. This was consistent with data from GVAX and standard treatments such as chemotherapy and radiotherapy: Macrophage presence correlates with poor survival.
Another observation was made by Ho and his team: There was an abundance of neutrophils in the PDAC microenvironment.
“We wanted to understand the role of these neutrophils when there is a strong antigen presence–strong immune-recognition,” he said.
Ho’s lab used the liver metastatic tumor microenvironment to investigate this question. The tumor burden remained the same despite whether the antigen was on or off. However, when the immune profile in the microenvironment was evaluated, there was a marked infiltration of neutrophils in the antigen-on tumor. Using laser capture microdissection and RNA sequencing, Ho’s lab observed the upregulation of chemokine ligands and chemokine signaling both in the cancer cell itself and in the cells’ surrounding vicinity.
“The cancer cell in its interaction with the immune response to the antigen, it’s upregulating these chemokines,“ he stated. “It’s also signaling to its adjacent cell to also upregulate the recruitment of neutrophils.”
Surprisingly, blocking the CXCR2 in mice with the antigen on setting results in smaller tumors but comparable amounts of neutrophil infiltration. When the mice were treated with drugs that stripped them of the neutrophils, Ho found that neutrophils were important to resisting the tumor. Sequencing of the neutrophils revealed high expression of the neutrophil subtype IV that was highly enriched in Mpo and Nos2 and expressed low CXCR2. To validate this finding, Ho evaluated in-vivo vaccinated PDAC samples (highly antigen-on) and found the same neutrophil subtype.
To further increase efficacy and clinical relevance for immunotherapy, Ho investigated the possibility of multi-pronged immunotherapy targets. PTPN22 is the pathway of interest to Ho’s lab because it’s only expressed in hematopoietic cells. In cancer, PTPN22 expression is associated with inflammatory cells and immunoregulatory genes.
Looking at a germline variant of PTPN22, however, Ho’s team found that the line is associated with a lower risk of cancer. To further explore the association, he investigated the signaling pathway in heavily immune-resistant PDAC.
“When we aggregated PTPN22 out of the mice, [we found] no signal there in terms of tumor growth resistance. When we actually used anti-PD1 therapy, what was really nice to see is that all of a sudden the tumor was sensitive to anti-PD1 therapy, and there was a 40% reduction in tumor growth,” he said.
From this observation and literature search, Ho hypothesizes that 41BB and OX40 agonists will synergize with anti-PD1 inhibition to set up PTPN22 aggregation in PDAC.
“There is now an 80%+ reduction of tumor growth when we combine 41BB co-stimulation,” Ho stated. “When we combine OX40 it’s a little bit busier… but the clear winner is PTPN22 being aggregated plus anti-PD1 and co-stimulation with OX40.”
Ho is trying to understand the mechanism underlying these phenotypes. His group found that degradation of TRAF3 (PTPN22 is structurally associated with TRAF3) induces translocation and enrichment of N22 at the membrane after 48 hours, which is a negative feedback loop that dampens T cell activation.
“If we get rid of that negative feedback we can further help the T cell activation. This is the insight that we are able to gain from this experiment[...] All this coming together as a T cell activation pathway when you aggregate PTPN22 and add the co-stimulation it’s really synergistic to push those T cells along,” he added.