A newly engineered cytokine/antibody fusion with promising clinical application was created and tested by a team at Hopkins. Their results were recently published in Cell Reports.
Antibodies are protective proteins that bind to and counteract substances that the body recognizes as foreign. Cytokines aid cell-to-cell communication during immune responses, such as signaling cells when to produce the appropriate antibodies.
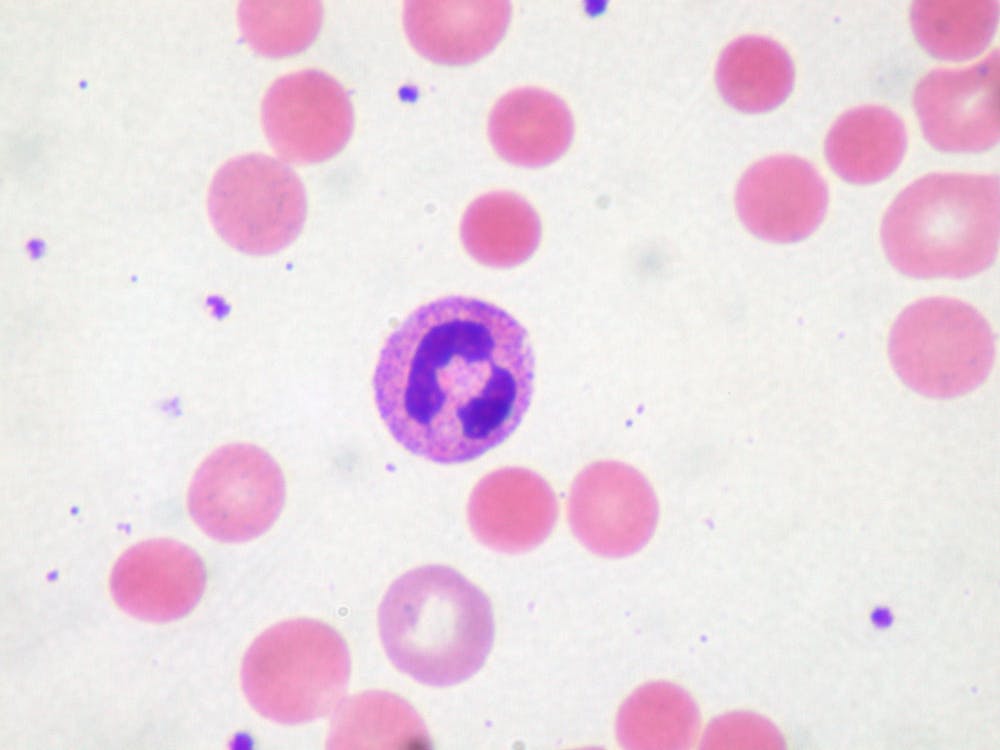
The team’s engineered cytokine/antibody fusion helps protect the immune system’s attack against itself when targeting autoimmune diseases by expanding regulatory T cells. Those protective cells suppress such autoimmune attacks. By acting together, the tethered antibody stabilizes the cytokine’s delivery and improves its performance.
The lead author, Derek VanDyke, explained the benefits of the team’s finding in an interview with The News-Letter.
“The single-chain nature of our molecule reduces off-target effects compared to other therapies, is more stable and is more clinically relevant,” he said.
Spangler is an assistant professor jointly appointed at the department of Biomedical Engineering and Chemical and Biomolecular Engineering. Her lab focuses on assembling natural molecules and designing new ones for immunology and disease prevention.
Spangler’s interest in this project sparked during her postdoctoral years when she determined the crystal structure of an antibody that binds to the cytokine interleukin 2 (IL-2) in mice. This preferentially activates regulatory T cells. The antibody in this project was originally co-developed by Jeffrey Bluestone and Pfizer in 2019.
Spangler discussed how the antibody influenced the cytokine in an interview with The News-Letter.
“The cytokine is already hard-wired in a certain way, and it is difficult to change. I learned that presence of the antibody can act as the cytokine's delivery vehicle and can modify its properties,” she said.
She was interested in examining the efficacy of the two molecules working together, both in optimizing the cytokine’s function and in localizing its impact.
VanDyke, who is a fifth-year PhD candidate in the department of Chemical and Biomolecular Engineering, facilitated the project when he joined Spangler’s lab in January 2019. After completing his undergraduate degree at the University of Massachusetts Lowell, he began working in Spangler’s lab developing antibody cytokine treatment for autoimmune diseases.
When coming to Hopkins for his PhD, VanDyke was excited about developing therapeutics and medicines.
“Much research has been done on cancer. I’m interested in the other end of the spectrum: autoimmune diseases. There is a huge clinical need for developing therapies for autoimmune diseases such as diabetes and multiple sclerosis,” he said.
VanDyke modeled the first design of the molecule within a few months of joining the lab. Optimization of the molecule followed and improved its efficiency in targeting specific suppressor cells and localizing its impact. The longest part of the process — working on the preclinical model — involved live animal studies, which required more time to obtain the the results of these tests.
Spangler praised VanDyke’s work on the project.
“To have gone from the conception of this molecule to an optimized drug candidate really speaks to Derek’s prolific work. The field of protein engineering has also come far enough to realize our objectives a lot faster than once possible,” she said.
IL-2, a cytokine that regulates immune responses, has been pre-clinically and clinically used. However, its limitation is that it activates both the suppressor cells (those that suppress autoimmune attacks) and the pro-inflammatory effector cells (those that reinforce autoimmune attacks). Without biased targeting of suppressor cells, IL-2 would experience reduced efficiency in suppressing autoimmune attacks, which is the goal in treating autoimmune diseases.
“Our molecule can activate specifically the suppressor cells. It’s important to have this specificity control in treating autoimmune diseases,” Spangler said.
The researchers recently patented their new molecule. They are currently looking for a pharmaceutical partner to develop their molecule into a drug and help them navigate regulatory considerations and marketing. The cytokine and antibody fusion will be further tested for clinical use. The team is also collaborating with researchers at Hopkins and other universities who are testing the cytokine and antibody fusion in new platforms and against specific autoimmune disease models.
VanDyke commented on the opportunity to see a project develop from its beginning to end during his time at Hopkins.
“Being able to take a molecule from design in theory to testing it in a preclinical model is really exciting,” he said.