Our brains are robust and highly efficient, tasked with managing our memories, emotions and identity. But what happens when this organ breaks down?
Xiaobo Mao’s team at the School of Medicine, which specializes in answering this question, published a paper in Nature Communications that details a potential treatment for neurodegenerative diseases like Lewy body dementia and Parkinson’s disease. The team’s findings focus on using nanobodies to disarm harmful protein clumps.
Ailments like Parkinson’s can cause unintentional muscle tremors, slowness of movement and, in later stages, difficulty performing automatic movements like walking and smiling. More frighteningly, no known cures exist for neurodegenerative diseases, except for treatments that can only slow the progression of severe symptoms.
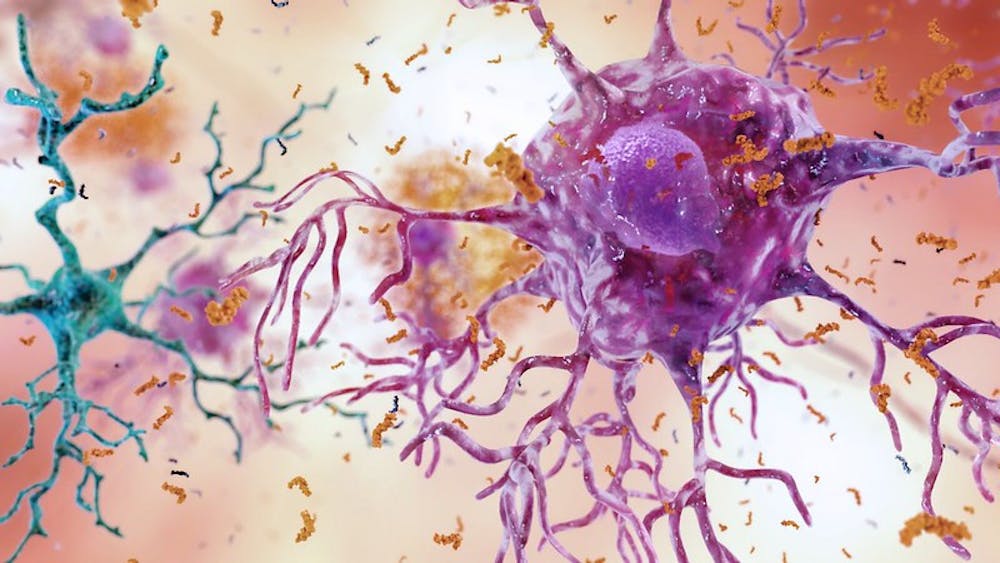
Researchers searching for a more effective cure have focused their efforts on α-synuclein, a naturally-occurring protein that is vital in transporting molecules around the brain. Issues arise when these proteins clump together, forming intractable aggregates called Lewy bodies. Scientists suspect that treatments that can mitigate this aggregation hold promise.
Past attempts have used antibodies, the more well-known protein that fits around harmful alien proteins like a glove. However, this approach for Lewy bodies has not worked well.
Ramhari Kumbhar, a postdoctoral fellow at the School of Medicine and the first co-author of the publication, discussed the team’s new approach in an interview with The News-Letter.
“The advantage over antibodies is that [nanobodies] are smaller in size and, most likely, easier to penetrate,” he said.
The Mao lab further designed a synthetic, disulfide-bond-free version of nanobodies, which is more stable than the conventional type.
In collaboration with the Wang lab at the University of Michigan Life Sciences Institute, Kumbhar and the team screened nanobodies to determine which ones would best fit the α-synuclein aggregates, like a clothing store fitting room but for the immune system.
Ultimately, according to Kumbhar, Nanobody Two was chosen to be the focus of the study.
“Two nanobodies showed very specific binding to the α-synuclein. It was PFF [preformed fibrils or ‘clumps’ of α-synuclein] Nanobody Two and Seven, but we did not include Seven in the study because it had nonspecific binding to other proteins,” he said.
The researchers used phosphorylation, the process of attaching a little glob of phosphorus, hydrogen and oxygen to a protein, as a marker to reveal α-synuclein gone wrong; an altered amino acid at position 129 is a common sign that α-synuclein is becoming toxic.
Kumbhar explained the team’s observations.
“In a control condition without nanobodies, you could see there was a lot of phosphorylation… but when we added nanobodies, it decreased,“ he said.
By measuring the level of synuclein phosphorylation in the blood serum, the team formed a metric to study the effectiveness of the nanobodies.
Testing progressed in phases. First, they used biochemical tests in vitro to test the nanobodies. After isolating and culturing cortical neurons from mice, they added the nanobodies and synuclein to the mix.
In vivo testing using animal models followed the initial in vitro tests. Kumbhar’s team at the School of Medicine employed the infecting capability of adenoviruses (similar to the ones in many COVID-19 vaccines) to deliver the nanobodies to the brain. Viruses containing nanobody genetic code would travel from the ventricular region to the brain and express the nanobodies directly.
Kumbhar noted that optimizing this method is one possible direction for future study. More work must be done to increase the efficiency of expression and coverage around the brain.
“This was just a proof of concept. Our next plan is to check what happens in adult mice,” he said.
The uniqueness of this approach lies in its use of nanobodies. While there have been attempts to bind the aggregates, the Mao lab’s nanobody takes it one step further by dissociating them. The team’s treatment not only halts the progression of neurodegenerative diseases but can theoretically reverse them.
Though this therapeutic is a long way from being implemented for the public, it could be a game changer in a larger battle against Parkinson’s and other neurodegenerative diseases.