David Bennett Sr., who received the world’s first genetically modified cardiac xenotransplantation (a pig heart transplant, in this case) at the University of Maryland Medical Center in Baltimore, passed away on March 8.
Bennett, age 57, had been diagnosed with terminal heart disease and was ineligible for a conventional heart transplant due to prior noncompliance with treatment instructions. Before the transplant, Bennett was under the cardiac support of an extracorporeal membrane oxygenation (ECMO) machine, which pumped and oxygenated his blood for him.
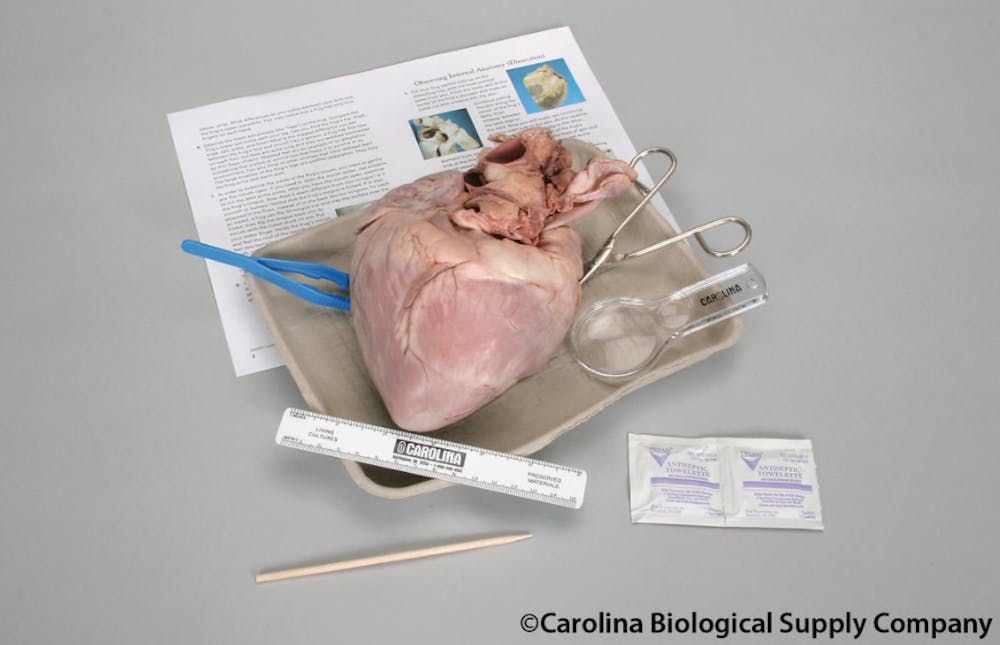
In an experimental procedure, granted emergency authorization by the Food and Drug Administration due to the rapid deterioration of his condition, a genetically modified pig heart was transplanted into Bennett on Jan. 7. Bennett’s condition eventually worsened, leading to his death two months later.
In an interview with The News-Letter, Dr. Ahmet Kilic, director of heart transplantation at the Hopkins School of Medicine, offered his perspective on the loss.
“It was really between a Hail Mary, in many regards, by undergoing this xenotransplantation or just dying, so in that way I don’t think you can really call the operation a failure,” Kilic said.
The xenotransplantation surgery was performed by Dr. Bartley P. Griffith, distinguished professor of transplant surgery and clinical director of the cardiac xenotransplantation program at the University of Maryland.
In working at the frontier of modern medical science, Griffith acknowledged in an interview with The News-Letter that questions are inevitably raised: of ethics, of practicality and of ensuring that what one is doing is not so much extreme as it is innovative. According to Griffith, the cornerstone of any such research is a fundamental concern for the patient.
“The only reason I am where I am is because of patient empathy. It has always been centered around the patient,” Griffith said. “Everything I do in the laboratory is simply a manifestation of frustrations over patient losses or patient difficulties.”
On Bennett specifically, Griffith explained the lengths that he and his team went through to ensure that everything, from the surgery to ethical considerations, was handled with caution and care.
“The prognosis without the transplant was thought very unlikely to extend beyond a few weeks,” he said.
The xenotransplantation was not the first attempt to replace human organs with animal substitutes. In 1964, Dr. James Hardy transplanted a chimpanzee heart into a 68-year-old man who died less than two hours later. In 1984, surgeons at Loma Linda University Medical Center transplanted a baboon heart into Stephanie Beauclair, a baby born with a terminal heart defect. Stephanie died 21 days later.
Griffith stated that tracking the field’s progress is more than just looking at strict binaries of success (the patient living) or failure (the patient dying).
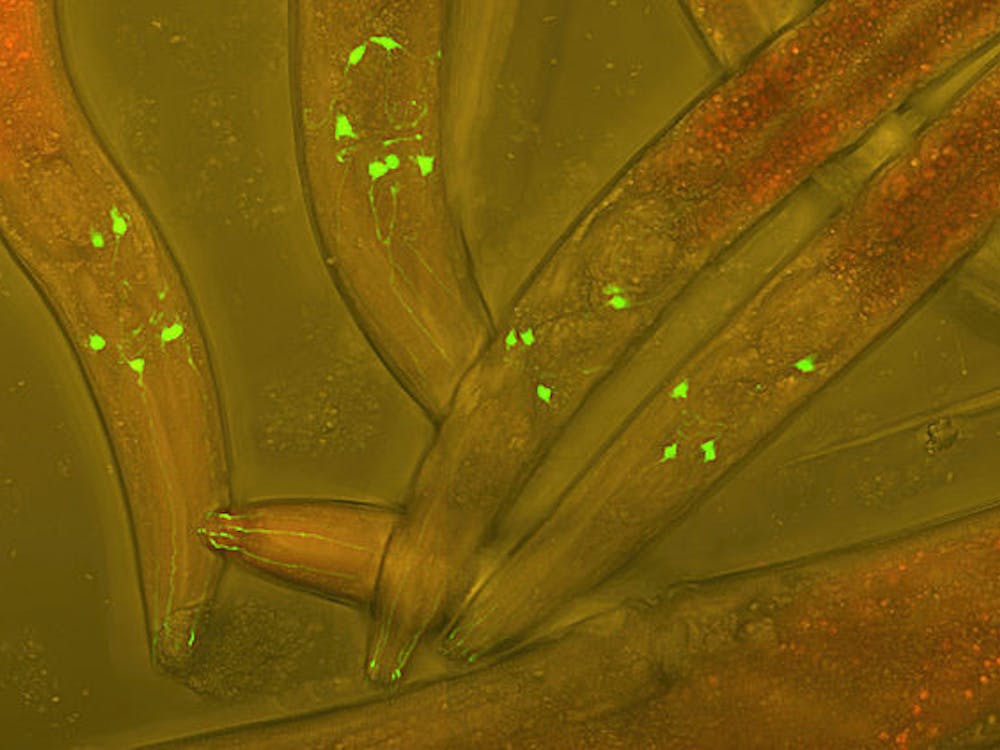
“It was incredibly sad when he died,” he said. “The Wright Brothers flew the airplane for a hundred yards, and we still celebrated. The public should know that we don’t just shoot a rocket to the moon and fly away; there are a lot of steps along the way. Realistically, this was a success. We are learning tremendously along the way, [such as] what we learned from when David was alive and what we can learn now from his tissues.”
Transplants like Bennett’s hold great promise for revolutionizing health care in a world where 8 to 15% of patients who need heart transplants die on organ waiting lists. With the abundance of animal hearts available, xenotransplantations offer utopian visions of forgoing the need for human donor hearts. Griffith cautioned against these idealistic notions while offering an outlook on the future of xenotransplantation.
“Unlike maybe the public’s view of it, this is a much more complicated problem to deal with,” Griffith said. “But having made a tremendous amount of progress with [Bennett], we can now look at this as a legitimate area for future progress. For humans, I think we are about five years away from a more regular opportunity to see this procedure performed in a larger number.”
Questions also arise about feasibility and whether resources might be better spent elsewhere. One argument says that instead of spending money on end-of-life treatments with limited success, money should be diverted instead towards prophylactic care that prevents the disease from ever occurring in the first place. However, Griffith argued against the notion that more money will automatically lead to a cure while acknowledging the importance of both avenues of thought.
“I actually believe more money needs to be going into both of these things. It’s an age-old response to new technology in medicine,” he said. “We have been trying to cure end-stage heart disease for a long time, just as we have been trying to cure cancer, but I think we all know that the silver bullet is not likely to occur any time soon. So I think along the way, it is appropriate to develop tools to help people live longer, before a cure is available. I think we can do both.”
Griffith cited the case of Dr. Lewis Thomas in particular, an acclaimed medical philosopher and physician who once remarked that the artificial heart was a “halfway technology” in that it only went halfway toward actually solving the underlying heart problem. However, Thomas later in life required a pacemaker for a heart condition, writing, “Here I am, enjoying precisely this sort of technology, eating my words,” and referred to the device as a “magical metronome.”
“It’s all in the eyes of the beholder,” Griffith said. “It’s easy to make those claims, and it’s usually made by people who have a fair amount of ignorance in the field they’re criticizing. And their criticism is very welcome; it’s what makes the world go round. But if every nickel that was spent on a chemotherapy treatment that didn’t work was instead funneled elsewhere, would we have a cure for cancer? I doubt it.”