Hopkins researchers have begun using Raman spectroscopy, a light scattering technique typically confined to the chemistry laboratory, in order to determine whether a patient will be a suitable candidate for immunotherapy.
Published in Cancer Research, the project is a joint collaboration between the Hopkins Department of Mechanical Engineering and the University of Arkansas Department of Biomedical Engineering. The project is helmed by Ishan Barman, associate professor of mechanical engineering at Hopkins with a joint appointment in the Sidney Kimmel Comprehensive Cancer Center.
Barman elaborated on the partnership in an interview with The News-Letter.
“Collaborations are typically driven by research interests and complementary competences. You don’t collaborate with people because they are sitting next door,” he said. “While being at Hopkins provides me with a wide array of wonderful clinical collaborators and bench investigators, this is one project where we work with the University of Arkansas and we’ve tried to see what comes out of that.”
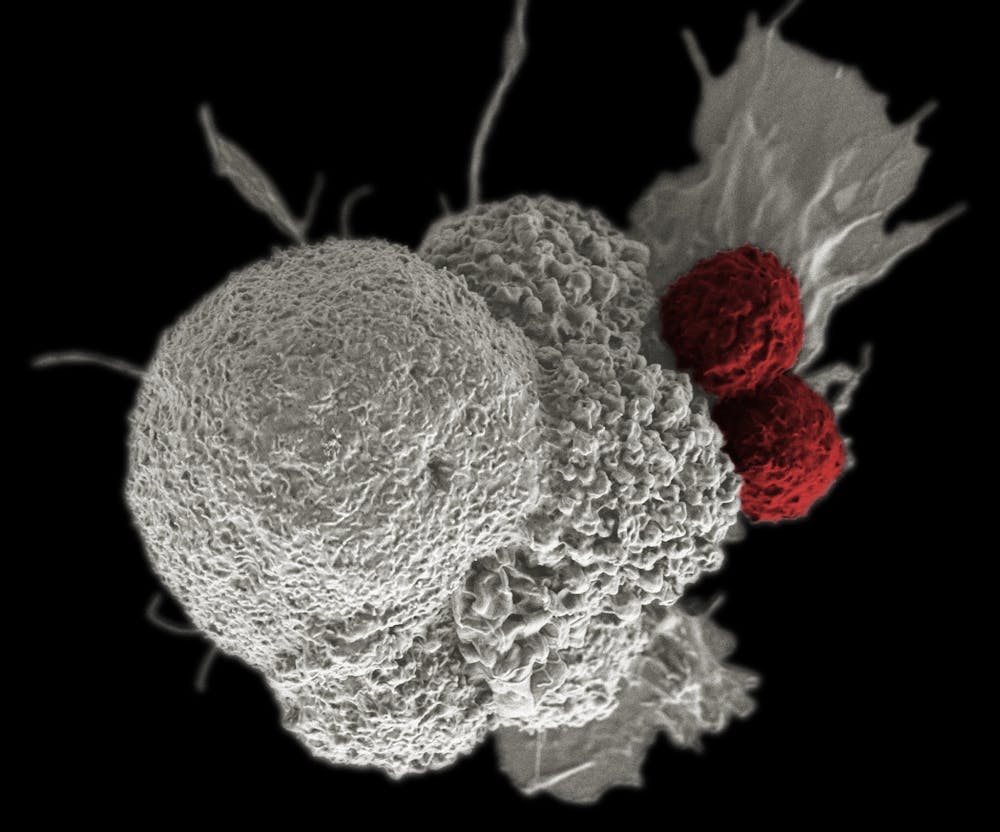
The project is another advance in the burgeoning field of immunotherapy. The discovery of cancer therapy through immune system regulation won the Nobel Prize in Physiology or Medicine in 2018, and immunotherapy has been heralded as one of the frontiers in the battle against cancer, allowing scientists to take advantage of the body's innate immune system to treat disease.
Barman discussed the profound impact of immunotherapy.
“Immunotherapy has revolutionized cancer treatment,” he said. “No other advance has had as dramatic an effect in the last five to six decades.”
However, one of the issues with cancer immunotherapy is that it is only viable in a relatively small percentage of patients. Being able to reliably identify this subset would allow doctors to treat patients with a greater degree of both precision and speed, preventing patients from receiving potentially harmful treatments that they don’t need.
Researchers can characterize the body’s different cancer biomarkers, tumor-specific molecules, to predict whether patients will respond well to immunotherapy. Current methods are still in the preliminary-results phase or have been shown to have little clinical benefit.
Barman explained how these limitations inspired his research.
“This study was really motivated by the lack of reliable predictors to immunotherapy response,” he said. “Standard treatment responses in the cancer space are measured by tumor size, and immunotherapy has actually come in and excluded this method.”
In the Barman laboratory, the key to demystifying these biomarkers involved looking into the microenvironment of the tumor itself and the many interactions that are taking place between the tumor and its surroundings, including blood vessels and nearby tissues. But the question remains: Which technique is best for examining the tumor microenvironment?
Enter Raman spectroscopy, an optical spectroscopic technique whose first observation dates back to 1928. Raman spectroscopy takes advantage of the inelastic scattering of light to determine a molecule’s vibrational mode, thereby revealing its structure. Although the technique is normally reserved for use in chemistry, it has enjoyed recent employment in the life sciences due to its remarkable specificity and ability to keep specimens alive. However, until Barman’s publication, no studies had been recorded detailing the use of Raman spectroscopy in understanding the responses of tumors to immunotherapies.
Barman reflected upon this relationship between engineering and the life sciences and the different perspectives that he is able to bring to projects.
“Many researchers within the clinical laboratories at the [School of Medicine] will readily admit to you that these kinds of tools are something that they are not familiar with,” he said. “But at the same time, it is not their job to be developing these tools; look at [who invented the] X-ray or even the microscope, which [are] now ubiquitous in any biology lab. We [engineers] are charged with creating what will become the next-generation tools for other scientists; I see this as a beautiful complement.”
To understand the effectiveness of the technique, mice were injected with tumor-producing cells and then subjected to Raman spectroscopy after having received immunotherapy. The data was then analyzed using a machine-learning model devised by Barman and his team. By looking at the subtle changes in spectroscopic data, they were able to characterize the response of the tumor microenvironment to immunotherapy.
Barman’s team offers data consistent with the idea that the tumor microenvironment is important immunotherapy. Future directions include the optical spectroscopic analyses of multilayer approaches that combine immunotherapy with other treatments such as chemotherapy or even combinations of different immunotherapies.
In researching these complex biophysical methods, Barman is well aware of the types of challenges that arise.
“Whenever you move into uncharted territory, there are some knowns and unknowns, problems you can predict and problems you would never expect to come up,” he said. “The main challenge [in this study] was, ‘How do you get people on the clinical side onboard for this proof-of-concept idea?’ Because there is certainly a degree of difficulty in getting the right amount of expertise on board.”