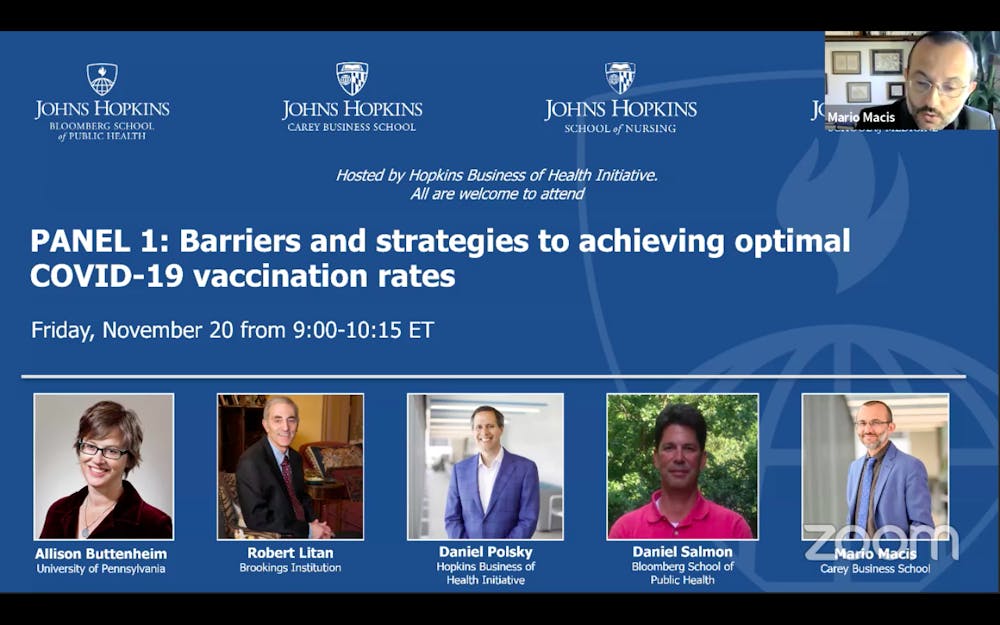
The COVID-19 Symposium, held by Hopkins Business of Health Initiative (HBHI), featured a segment titled “Financial incentives and disincentives for achieving optimal COVID-19 vaccination rates” on Friday. A panel of experts in the fields of behavioral sciences, public health and economics discussed barriers and strategies to maximize COVID-19 vaccination rates. The discussion was moderated by Mario Macis, professor of Economics at the Hopkins Carey Business School.
Alison Buttenheim, associate professor of Nursing and Health Policy and scientific director of the Center for Health Incentives and Behavioral Economics at the University of Pennsylvania, explained the current situation from a behavioral scientist’s view. Buttenheim categorized the 50% of the population who might refuse to receive the vaccine into three groups.
The first group is the anti-vaxxers, who have exerted a strong presence through social media despite being a relatively small group. Unfortunately, due to their strong and unwavering beliefs, it is unlikely to convince them to receive the vaccine.
The second group consists of 20 to 40% of the entire U.S. population who are hesitant about the newly developed vaccine and are vulnerable to misinformation.
The third group is those who are neutral or motivated to take the vaccination yet there exists a gap between their intention and behavior.
Professor Daniel Salmon, director of the Institute for Vaccine Safety at the Bloomberg School of Public Health, raised additional difficulties the field of public health is facing to encourage vaccination.
Salmon described how there is significant mistrust in the government and public health institutions. However, this mistrust did not arise due to COVID-19. Instead, it has been deeply rooted in the society before the pandemic, with one out of three parents hesitant about vaccination.
“[The mistrust] speaks to how pervasive these issues were in the society before COVID,” Salmon said.
Daniel Polsky, Bloomberg distinguished professor of Health Policy and Economics and director of HBHI, listed financial obstacles in obtaining the new vaccine.
Polsky described how vaccines purchased with U.S. taxpayer dollars will be offered free of cost to Americans, but not all vaccines are purchased by taxpayer dollars. Additionally, an administration fee may apply. While the administration fee may be covered with health insurance, reimbursement through health insurance or a relief fund may not fully cover the costs.
After identifying societal barriers, the panelists introduced strategies dedicated to reaching a high rate of vaccination.
Although little can be done to change the mind of anti-vaxxers, behavioral science strategies can still focus on the two other groups to convince them to receive vaccination. Buttenheim suggested that communication tactics are helpful in this case. The goal is to send the U.S. population a message expressing that vaccination is an easy and safe process.
“We want to make this as easy as possible for people to get vaccinated. We want this to be a zero-friction, zero-hassle, zero-cost process,” Buttenheim explained.
In addition to the clarification on the vaccination process, Buttenheim also recommended making vaccination a social norm. Specifically, she suggested having public figures — chief executive officers, mayors and celebrities — receive the vaccine to lead a trend favoring vaccination.
She described how just as “I voted” stickers are a public incentive to vote, “I vaccinated” stickers can become a signal for participation in social good. Health agencies can also take advantage of the supply limit of the vaccine. As people put more value on things that are harder to obtain, this mentality could be utilized to prompt precommitment to vaccination.
However, Buttenheim recognized that tests, results and strategies for different target groups are necessary before a final plan can be established.
“It’s an exciting time to be a vaccine-acceptance researcher and a behavioral scientist. [I am] looking forward to that challenge,” Buttenheim added.
In contrast to Buttenheim’s optimism, Salmon believes that a mass-communication campaign will not be sufficient enough to solve the problem. Instead, different strategies and messages need to be directed towards communities.
“We need to know what the population thinks about the disease and about the vaccine. We need to know how it varies by some population. We need to know what credible sources are among those subpopulations. And then we need to know how to message within those individual areas,” Salmon concluded.
In order to resolve the problem of possible costs for the COVID-19 vaccine, Polsky stressed the importance of sufficient reimbursement through health insurance companies. Also, more relief funds are needed to abundantly cover the uninsured 30 million individuals in the United States.
“We want to make payers accountable for adequate reimbursement rates, especially in harder-to-reach places,” Polsky said.
Robert Litan, a nonresident senior fellow at the Brookings Institution, proposed a backup plan.
Litan proposed that the federal government needs to provide financial incentive for vaccination. This proposal would theoretically only come into play when all the other strategies described fail to produce an effect.
In his proposal, all individuals would receive $200 at the time of vaccination. An additional $800 would be given after the required coverage of vaccination in individual communities for herd immunity is reached.
$1,000 per person for 60 to 70% of the entire U.S. population is a significant number. However, Litan argues that this money distribution is in fact a “booster shot” for the economy. The goal is to return society back to normal as soon as possible.
Some raised concerns that a financial incentive might suggest to the public that the vaccine is dangerous. Litan replied that with a large enough disbursement, the population can hopefully ignore the risky signal.
“We all know from the proverb that it is much easier to get people to change their mind through honey rather than vinegar. The honey is the financial incentive,” Litan said.
The four panelists identified barriers and solutions through their various fields of expertise. Interestingly, all four panelists agreed that no matter which method is taken, a larger federal budget is required to incentivize the public to vaccinate.