The Osler Medical Symposium and Conversations in Medicine co-hosted an event titled “Hand, Face, Genital Transplants” on March 22. The two organizations are student-run lecture series focused on issues in health care and medicine.
The two speakers featured at the event were Dr. Gerald Brandacher and Jeffrey Kahn. Brandacher is the scientific director of the Reconstructive Transplant program at the Hopkins Hospital and is also an associate professor of Plastic and Reconstructive Surgery at the School of Medicine. Kahn is the director of the Berman Institute of Bioethics. He is also a professor of Bioethics and Public Policy in the Department of Health Policy and Management in the Bloomberg School of Public Health.
In their talks, the speakers discussed the ethics of vascularized composite allotransplantation (VCA) compared to solid organ transplants and the implications for donors, patients and their families.
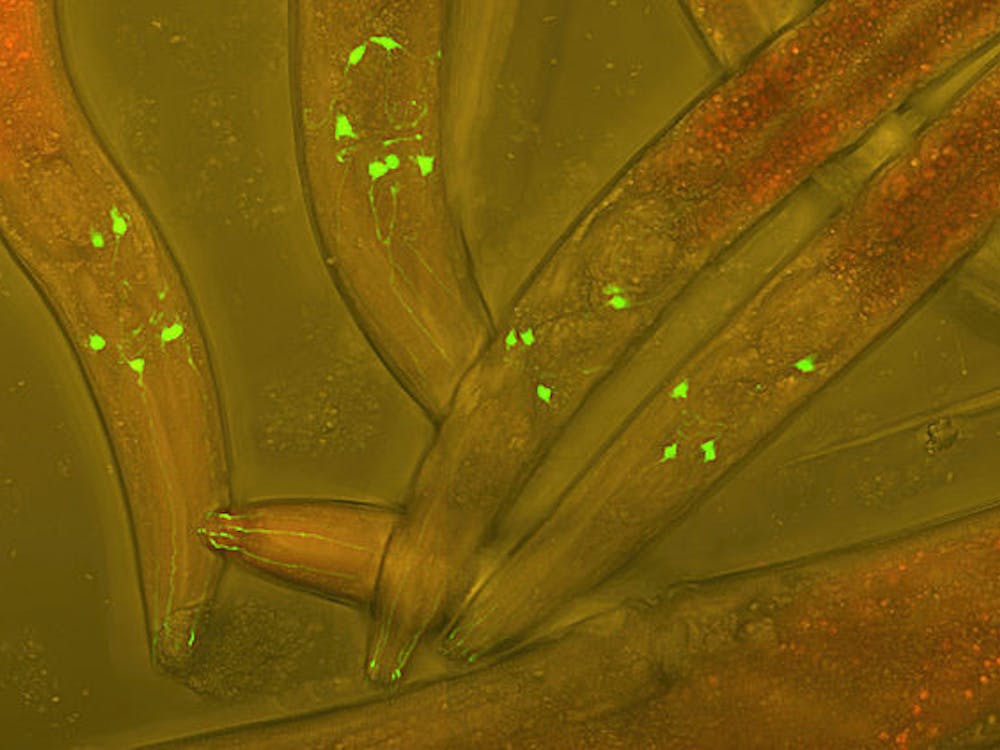
VCA refers to the transplantation of a functional unit, such as a hand, face or genitals. Since the whole unit is transferred, the procedure involves the transplantation of multiple tissues like muscle, bone, nerve and skin.
Traditional transplantation procedures are termed solid organ transplants; these operations involve the transplantation of organs such as the kidneys, heart, liver and lungs.
According to Kahn, medical professionals have to weigh the risk-benefit surrounding VCA, which is a life-improvement operation, differently than a life-saving operation like a solid organ transplant.
Brandacher was a part of the medical team at the Hopkins Hospital that performed the first successful penis and scrotum transplant. He explained that the screening process for a VCA in particular is very involved. The patients undergo a thorough work-up which examines the technical and psychosocial feasibility of the operation.
“We figure out if the surgical aspect will work, which is probably the hardest part of all,” Brandacher said. “We need to make sure that [patients] understand fully that the transplant will last for the rest of their life, and that they have realistic expectations in regards with functional outcomes.”
Kahn noted the difficulty in determining realistic expectations for patients while emphasizing that such expectations are critical for the patients and their families.
“It’s not clear that people can understand what their expectations ought to be as a result of these operations. There have been too few operations done to give people a sense of what their expectations ought to be,” he said.
The novelty of the VCAs also affects what is deemed the appropriate level of consent from the patient undergoing the procedure. Especially in the case of the first face transplant, which Brandacher discussed in his presentation, Kahn argued that adequate consent was difficult to measure because there were no prior results for the patient to use to make an informed decision.
Given these ethical concerns, Kahn commended the Hopkins medical team for seeking the advice of experts in the Berman Institute throughout the process.
“We have been extraordinarily careful here at Hopkins, to the credit of the medical team who reached out to my colleagues to help them in these issues,” Kahn said.
Complex ethical questions are not limited to the patients receiving the transplant. The donation of the transplants have also been scrutinized.
When people go to the Department of Motor Vehicles (DMV) to renew or receive a new license, they are typically asked if they want to be organ donors. Kahn questioned the rigor of the process to be considered an organ donor. With the rise of VCAs, is a blanket statement at the DMV enough? Or should there be conditional terms of organ donation such that special requests must be made for certain kinds of transplants, specifically those involving external organs? VCAs can be particularly sensitive since the external organs can be seen by a donor’s loved one. Open casket burials may also pose a problem for donor’s families.
“We want to save lives, but we don’t want to undermine the life of the donor,” Kahn said.
At the Hopkins hospital, VCA is only considered after the patient tries a prosthesis for an extended period of time. But based on Brandacher’s experience, patients incorporate transplants into their body schema more easily than prosthetics.
“With a transplant, for all of our patients, the moment they wake up from surgery they refer to the hands as ‘my hands;’ we have never seen a patient say ‘transplant’ or ‘graft,’” he said. “They immediately integrate it into their body.”
Post-operation, the success of the transplant is difficult to quantify. According to Brandacher, one difficulty lies in the different expectations that patients have for the transplant: One may prioritize sensation while another may prioritize function.
“A patient may say that they only want to feel the touch of their daughter’s hand. For this patient, sensation is very important despite of the fact [that the hand] may not work at all. Another patient may say that they want to play violin or piano,” Brandacher said.
Brandacher reasoned that to determine success, qualitative research studies must be conducted. Kahn agreed and said that the development of a database on which both patients considering the procedure and medical teams can rely, is critical.
The future of VCAs remains as hazy as the present. According to Kahn, as VCAs become less novel the popularity of those procedures will increase. This will lead to new questions of which contexts VCAs should be administered. Should VCAs be used in cases of genital deformation or gender reassignment? In other words, what should be the limits of the conditions in which VCAs are acceptable?
Only the march of medicine will tell.