While many people hear “wearable device” and think about the smartwatch they have strapped on their wrist or the Fitbit tracker they use on their runs, wearables are now being used for medical purposes.
The newest version of the ubiquitous Apple Watch has a built-in electrocardiograph, also known as a medical heart-monitor, that is usually bulky and found only in health care settings.
Purdue University researchers announced on Oct. 16 the development of advanced wearable paper-based electronics. These epidermal, paper-based electronic devices (EPEDs) are inexpensive to manufacture and carry several advantages over traditional wearables.
An estimate by the Purdue team stated that the expected cost of manufacturing each EPED was under six cents. And because of their cellulose base, EPEDs are biocompatible and can conform to the shape of internal organs, allowing for more comprehensive diagnostics and monitoring without fear of rejection.
Biomedical engineer Jessilyn Dunn from Stanford University wrote a paper about the uses of wearable sensors, published in Future Medicine.
“Wearable devices (wearables) are already revolutionizing biomedicine through mobile and digital health by enabling continuous, longitudinal health monitoring outside of the clinic,” Dunn wrote in her paper.
These devices, particularly those dedicated to medical applications, allow tracking of vital signs, bodily functions and bioelectrical activity, according to Dunn.
Additionally, one-in-six consumers in 2013 owned some type of wearable device, according to a Nielsen survey, and since then, that number has surely increased. This statistic suggests that Americans are not averse to wearing smart health trackers.
But where Apple Watches, Fitbits and other consumer wearables usually carry price tags of over a hundred dollars, by using paper as a substrate, EPEDs can be produced for far less and can be manufactured at high volumes.
Beyond the affordability factor, the Purdue researchers explained in a research paper published in Applied Materials & Interfaces that paper is breathable and easily available in a wide variety of densities and thicknesses.
However, the researchers went on to say that paper-based electronics are affected by environmental humidity. This would preclude the use of EPEDs on an everyday basis, which is the primary goal in consideration, as EPEDs should ideally be able to withstand as much as the outer skin layer does.
To address this flaw, the Purdue team attempted to use omniphobic paper coated in fluoroalkylated trichlorosilanes that would prevent water and organic liquid damage.
Spraying the paper with long-chain fluorinated organosilane allows more-than-adequate breathability, while preventing liquid damage to the circuitry. However, RF paper, as it is called, does not adhere well to skin and is nowhere near as stretchable as would be requisite for a device worn every day.
The researchers, upon encountering these barriers to designing a successful EPED, found several workarounds, as published in the aforementioned paper.
To attach the RF paper to skin, they used water-soluble tape to facilitate the paper and circuit’s transfer onto skin before being dissolved.
After the dissolution of tape, previously-applied medical glue will hold the paper in place. They also greatly increased the stretchability of the stickers by laser cutting the layout of the EPEDs in an “open mesh serpentine design.”
The implications of such a technology are massive. Beyond simple vitals tracking, EPEDs could be used in medicine from cancer to the brain.
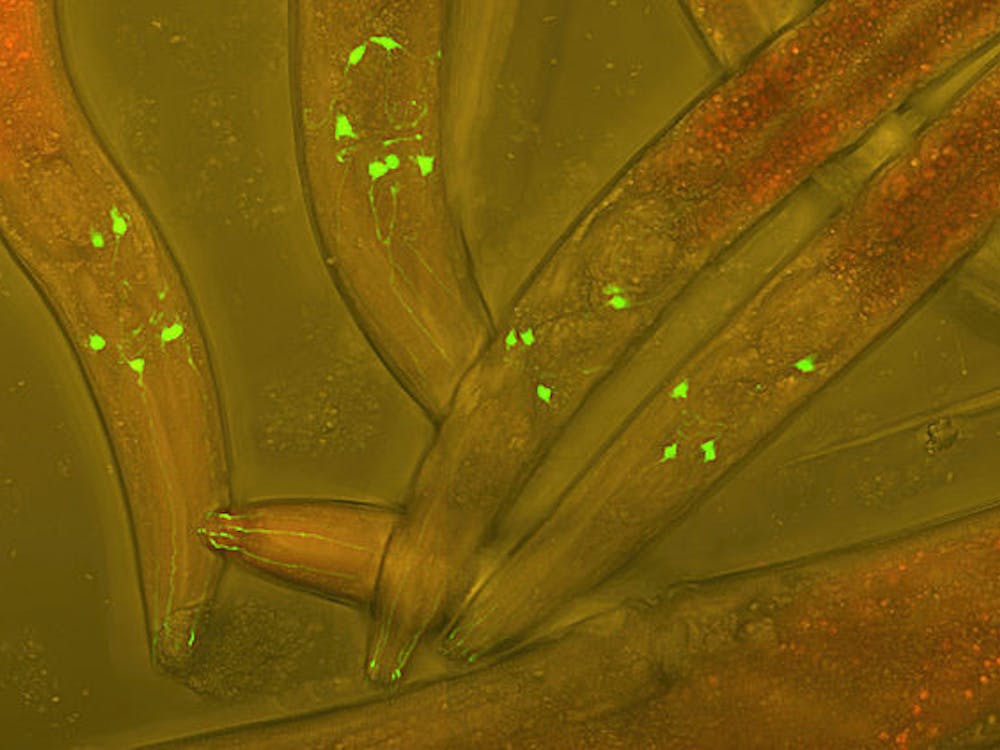
Because EPEDs have been shown to be compatible with “wireless powering via inductive coupling,” they can potentially allow for hyper-localized thermal cancer therapy, a novel form of cancer treatment by Joule heating. EPEDs could also hold significant promise in optogenetic applications, a process where light is applied to selectively control neuronal activity. But one thing is certain: The possibilities are practically endless.