In human diseases and injuries, inflammation is a critical defense and repair mechanism. In response to a physical injury or infection, immune cells are recruited to the site of inflammation to defend against the foreign injury or pathogen. However, immune cells also have destructive properties. Persisting inflammation can create an opposite effect, causing more harm than benefit.
The bone marrow, a soft, spongy tissue in the center of most bones, produces both red and white blood cells. While the bone marrow is known to release white blood cells after an injury, it is unknown whether its activity is homogeneous throughout the entire body.
Researchers at the Harvard Medical School and Massachusetts General Hospital lead by Dr. Matthias Nahrendorf recently addressed this gap in knowledge using state of the art cell-tagging and tracking techniques. Their results were published in Nature Neuroscience.
Nahrendorf serves as the Director of the Mouse Imaging Program at the Center for Systems Biology. His research interests focus on the imaging of molecular processes during the healing phase after heart attacks.
Using mice models, Nahrendorf’s research group initially found that skull bone marrow contributed more neutrophils, immune cells that arrive at earlier stages of inflammation, compared to leg bone marrow.
By observing the migration of immune cells, the population of neutrophils in the skull six hours post brain injury was significantly lower than those in the leg bone marrow, reflecting that there was more contribution and release of immune cells from the skull compared to the leg bone marrow.
Furthermore, the researchers began to decipher the mechanism underlying this differential release by comparing SDF-1 levels.
SDF-1 is responsible for keeping white blood cells inside the bone marrow. A significant decline in SDF-1 levels was found only in the skull after stroke in the brain, which supports the previous finding on preferential release of neutrophils.
This discovery led the research team to examine the skull in more depth to understand the pathway neutrophils use to reach the injured brain.
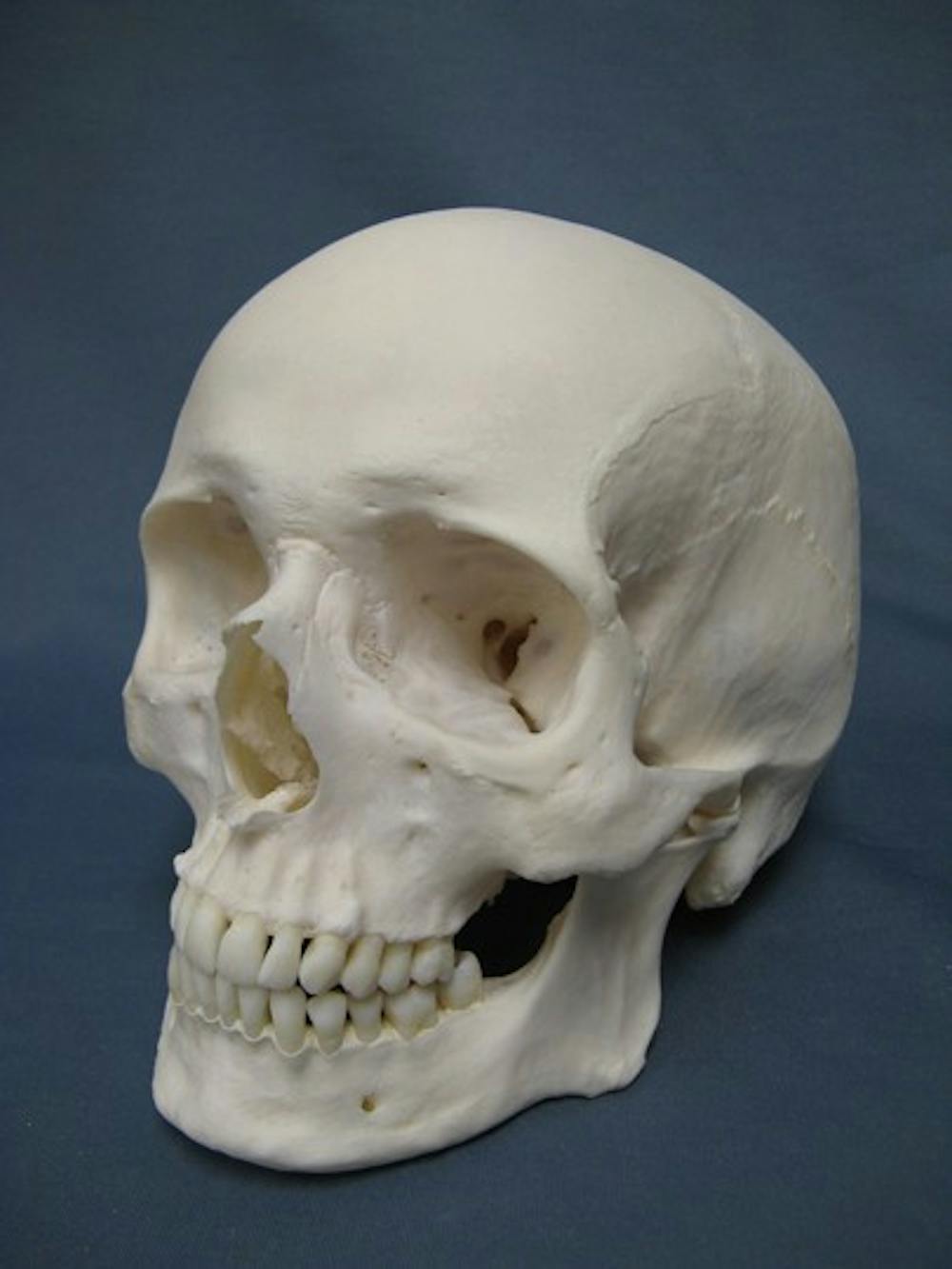
“We started examining the skull very carefully, looking at it from all angles, trying to figure out how neutrophils are getting to the brain,” Nahrendorf said in a press release. “Unexpectedly, we discovered tiny channels that connected the marrow directly with the outer lining of the brain.”
Not only was this channel found in mice, but humans were also identified to have similar channels. The channels found in humans were 5.3 times larger in diameter compared to those found in mice.
These results challenge the conventional notion that after any inflammatory stimulus, all bone marrow homogenously release white blood cells into the circulation system.
“We always thought that immune cells from our arms and legs traveled via blood to damaged brain tissue. These findings suggest that immune cells may instead be taking a shortcut to rapidly arrive at areas of inflammation,” Francesca Bosetti, program director at the NIH’s National Institute of Neurological Disorders and Stroke (NINDS), said in a press release.
Bosetti adds that this novel discovery is full of potential, capable of opening new doors in inflammation-related research.
“Inflammation plays a critical role in many brain disorders and it is possible that the newly described channels may be important in a number of conditions. The discovery of these channels opens up many new avenues of research,” Bosetti said in a press release.
This research poses several more interesting questions waiting to be explored, such as the functional role of these channels and how these channels are regulated under different intracranial pressures.