Researchers at the University of Lincoln have discovered a new class of natural antibiotic drugs that is predicted to dramatically affect the battle against bacterial infections.
According to the Centers for Disease Control and Prevention (CDC), approximately two million people are infected with antibiotic-resistant bacteria each year. Furthermore, approximately 23,000 people die from these untreatable infections.
Bacterial infection is the proliferation of harmful microorganisms that can be stopped by antibiotics. Antibiotics work by targeting structures in bacterial cells that human cells do not possess, such as a peptidoglycan cell wall. Bacterial cells need a cell wall in order to survive; as a result, its functions can be compromised by preventing the bacterial cell from building a cell wall.
Antibiotics, like all other drugs, can be misused. If antibiotics are overused, the bacterium can become resistant to the antibiotics. Antibiotic resistance can also be transferred from one bacteria to another, causing not only that strain to be resistant but also different bacterial strains surrounding it.
Antibiotic resistant pathogens are microorganisms that have evolved through natural selection and are able to withstand the harsh effect of antibiotics. Methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) are two commonly known antibiotic-resistant strains of bacteria.
However, scientists at the University of Lincoln have recently synthesized a new class of teixobactin antibiotics capable of killing some of the previously antibiotic-resistant bacterial infections.
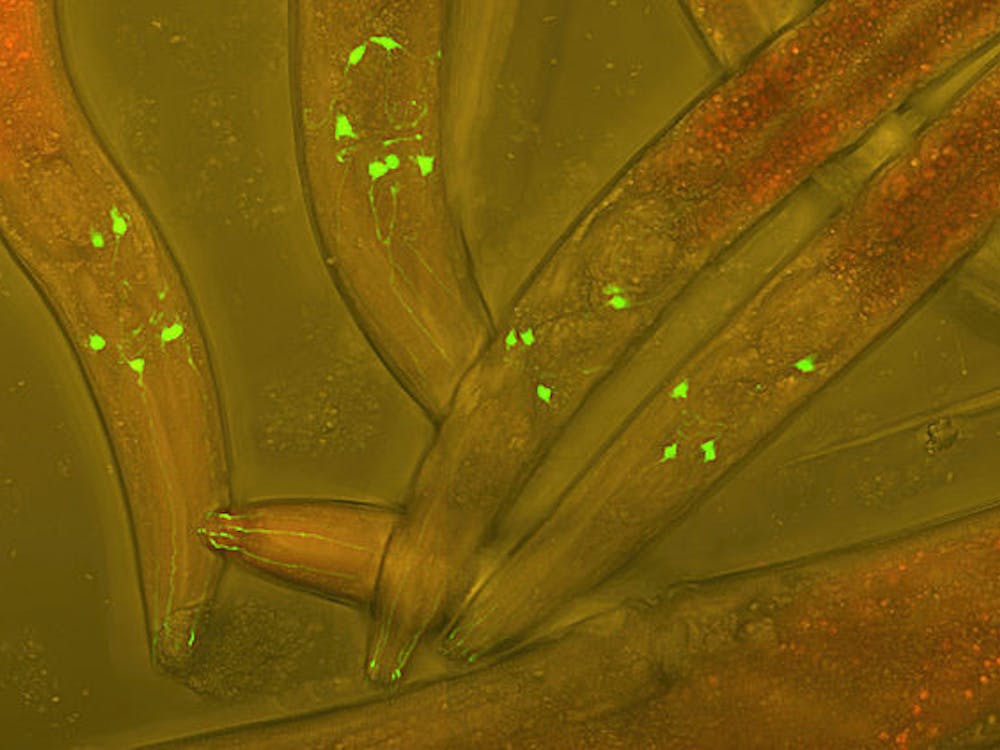
Teixobactin inhibits cell wall synthesis in bacteria by binding to lipid II, a precursor to peptidoglycan. In other words, teixobactin inhibits the production of the peptidoglycan layer in bacteria, causing the cell to disintegrate.
In an experiment run by researchers from the Singapore Eye Research Institute (SERI), mice with bacterial infections were able to be treated using the synthetic teixobactin. On top of that, the treatment also minimized the severity of the infection.
Teixobactin was found to be most effective against gram-positive pathogens, even antibiotic-resistant strains such as MRSA, VRE and Mycobacterium tuberculosis.
On the other hand, although teixobactin is ineffective toward most gram-negative pathogens, it proved to be effective for certain strains of Escherichia coli.
Rajamani Lakshminarayanan, a researcher at SERI, shared his views on the implications of the study.
“Drugs that target the fundamental mechanism of bacterial survival and also reduce the host’s inflammatory responses are the need of the hour,” Rajamani said, according to Sciencedaily. “Our preliminary studies suggest that the modified peptide decreases the bacterial burden as well as disease severity, thus potentially enhancing the therapeutic utility.”