Last week, researchers at the Stanford University School of Medicine published a study detailing how injecting pluripotent stem cells into the body may train the immune system to attack or even prevent cancer, thereby acting as a cancer vaccine.
According to the National Cancer Institute (NCI), 40 percent of all men and women will be diagnosed with cancer at some point in their lives. The United States spends nearly $150 billion on cancer care each year, yet cancer still claims 600,000 American lives annually.
The World Health Organization (WHO) reports that worldwide, that number increases to up to 10 million people annually.
Cancer is one of the leading causes of death around the world and is thus intensely researched. The past few decades have marked many successful treatments against the most widely studied cancers, such as breast cancer and colon cancer.
From regular exams for early detection to radiation treatment, targeted drugs and surgical intervention, the medical and scientific communities are rallying against the terrible disease. But to this day, there has yet to be a cure for cancer, or a way to prevent it for good.
One challenge is that cancer is extremely diverse. Cancer can occur in practically any tissue in the body and can grow at different speeds and levels of malignancy.
Much of a cancer’s onset and progression depends on the individual, since each person is genetically predisposed to different types of cancers and exposed to different environmental factors that may influence cancer development. In addition, everyone responds differently to treatment. Drugs that work potently on one person’s cancer may not work at all on another’s.
Despite the obstacles, breakthroughs like the one made by the cancer researchers at Stanford last week provide some hope.
It all began when the research team, led by Dr. Nigel Kooreman and Dr. Joseph Wu, discovered that induced pluripotent stem cells are in many ways similar to cancer cells.
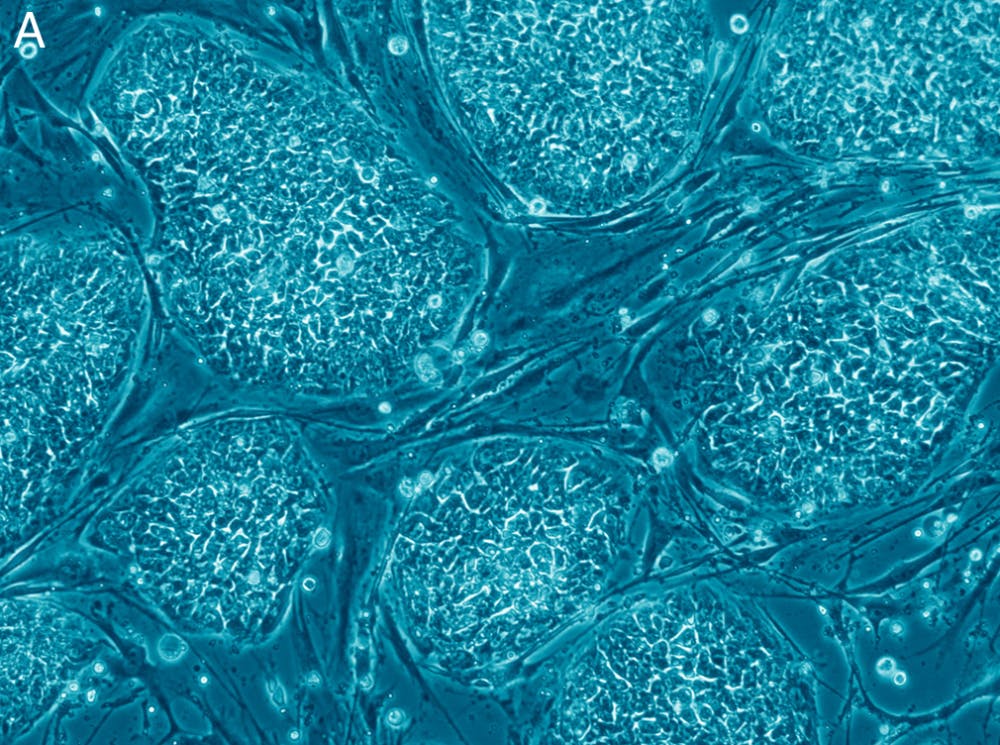
Induced pluripotent stem cells (iPSCs) are cells derived from adult fibroblasts (such as skin or blood cells) and are subjected to specific conditions that reverse their development to become pluripotent, meaning they can differentiate into practically any type of cell in the body.
iPSCs are widely used in research for personalized and regenerative medicine because they can be generated from a patient’s own blood cells.
This allows for the testing of different treatment methods on the patient’s own cells in culture or the growing of the patient’s own tissues that can be used for regenerative purposes without fear of implant rejection.
While studying iPSCs and cancer cells, Kooreman and Wu’s research team found that cancer cells, like iPSCs, are similar to developmentally immature cells.
Part of the normal cell to cancer cell transition involves the cell losing its ability to regulate cell division, the absence of which is characteristic of cells in their early growth stages.
Findings from research in gene expression also revealed close similarities between iPSCs and cancer cells, suggesting that the two cell types may share the same type of epitopes, or cell surface protein markers.
Based on this data, the scientists hypothesized that antibodies that recognize iPSCs would also recognize most cancer cells.
To find out, they conducted an experiment on four groups of mice: The first group was injected with a control solution and the second with the corresponding iPSC cells (irradiated to prevent the formation of tumors by the iPSC cells themselves) derived from each mouse’s own blood samples. The third group received a general immune system stimulant known as adjuvant, while the last group was injected with a combination of irradiated iPSCs and adjuvant.
After a mouse breast cancer line was transplanted into each mouse, the mice were injected with the experimental treatment once a week for four weeks.
One week into the experiment, all mice had developed breast cancer tumors. In the control group, the tumors grew potently. However, in seven of the 10 mice injected with the iPSCs and adjuvant combination, the scientists obseved the tumor shrink in size. In two mice, the tumor disappeared completely, allowing the mice to live more than a year after the tumor transplantation.
Furthermore, Kooreman and Wu found that immune system T cells taken from vaccinated mice slow the cancer growth of unvaccinated control mice following injection.
The team also used mouse melanoma (skin cancer) and mesothelioma (lung cancer) cell lines to confirm the data and obtained similar results.
With further research on human iPSCs and human cancers, the hope is to create a method that allows healthcare workers to draw blood from a patient and create a specialized treatment for that individual, one that stimulates the patient’s immune system upon reinjection to produce antibodies that can recognize cancers and attack them or prevent their formation. It could be used as a cancer vaccine or as treatment for an existing cancer in conjunction with other methods.
The advantage of this method is that the patient’s immune system would produce its own mechanisms to fight or protect against cancer, so it should function well for practically every patient.
It can also expose the immune system to the epitopes of different cancer types at one time, allowing quick response and defense from a variety of cancers the patient may develop.
In a interview with The News-Letter, sophomore Sehej Parmar spoke about her experience coping with cancer in her family.
Cancer runs in Parmar’s family. Parmar’s father is a survivor of two cases of stage three colon cancer. Her grandfather was diagnosed with stage four prostate cancer last year and passed away three months later. Last week, her grandmother was just diagnosed with stage two breast cancer.
“I am myself very likely predisposed to cancers. Though the usual age for regular colonoscopies at physical exams is 50, I will be starting them in less than two years to monitor for colon cancer,” Parmar said.
Parmar shared that she is really grateful for technology that increases the chance of early diagnosis or even prevention of cancers.
When asked about the potential of a cancer vaccine derived from iPSCs, she said that she believes the study is very promising. Parmar works in a cancer research lab at the Sidney Kimmel Cancer Center, and she finds cancer research fascinating mostly because she knows the purpose behind it is to help those struggling with cancer and to eventually prevent its onset entirely.
“I think preventive medicine, like the idea of a cancer vaccine, is the future,” Parmar said. “Cancer is so widespread and devastating, and even if a person survives cancer, it takes away years of carefree, happy living from them. Preventing it entirely would not only prolong life, but also increase life quality. It will allow people to live the life they want to live.”
Although further research is necessary, the battle against cancer may have just taken one step closer to victory.