A recent genome analysis of almost 3,000 individuals has provided more evidence that supports the theory that the mutation which causes sickle cell anemia may have originated from a single person, nearly seven millenia ago.
The study was carried out by Daniel Shriner and Charles Rotimi from the National Human Genome Research Institute at the National Institute of Health.
Sickle cell anemia occurs when two mutated copies of the hemoglobin gene are inherited.
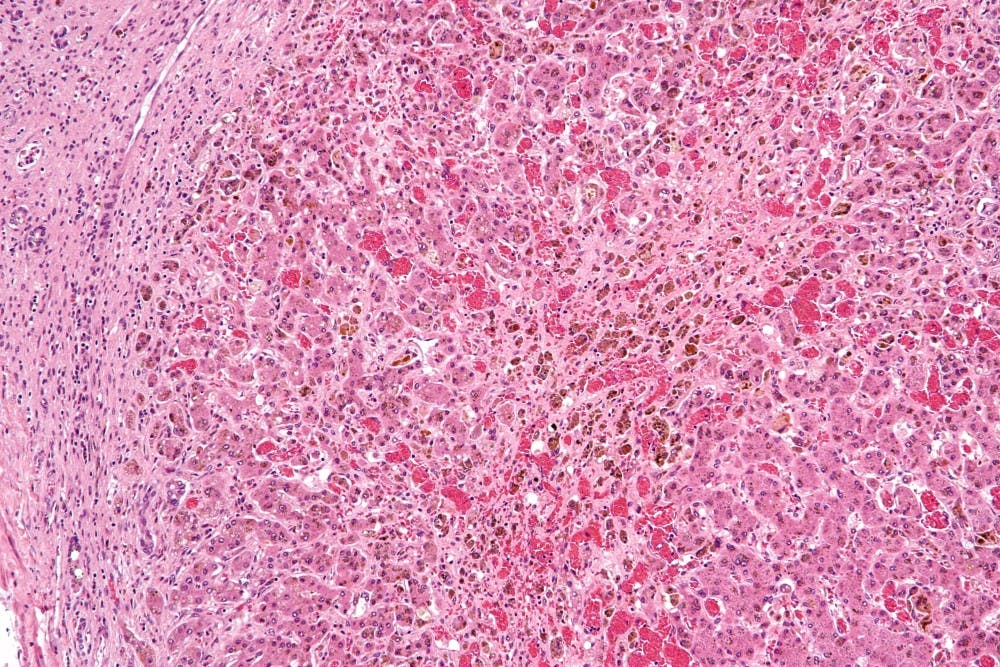
Hemoglobin is a protein found in red blood cells and is responsible for transporting oxygen, and individuals with the mutation produce an abnormal hemoglobin molecule called hemoglobin S. This results in red blood cells that are rigid and sickle-shaped, which can obstruct blood vessels.
Those who have, or are carriers of, sickle cell anemia most commonly have African, South American, Mediterranean or Arabian Peninsula ancestry.
Symptoms and complications of sickle cell anemia include swelling of the hands and feet, jaundice, anemia caused by the rapid death of sickled cells, sudden episodes of pain called “crises,” and organ damage from lack of blood flow.
While bone marrow transplants have been explored as a potential cure, treatment usually involves managing symptoms. In the United States, those with sickle cell anemia have an average lifespan that is almost 30 years shorter than the life expectancy of the general public.
There have been two theories about the origin of the sickle cell mutation.
One idea, the multicentric model, is that the mutation arose independently five times in different geographical locations. This hypothesis came from the observation of five classical sickle cell haplotypes, or groups of associated single-nucleotide variations.
These sickle cell haplotypes are named for the region or ethnic group the patients they were originally from: Arab-Indian, Benin, Cameroon, Central African Republic and Senegal.
In contrast, the unicentric model involves a single origin for the mutation. This is the hypothesis supported by Shriner and Rotimi’s study, which was published in early March. In the study, 2,932 whole genomes from the 1000 Genomes Project, the African Genome Variation Project and sequencing efforts in Qatar were analyzed. Of these, 156 had a copy of the sickle cell mutation.
The researchers defined new haplotypes using phased sequence data, as opposed to using restriction sites, through which the five classical haplotypes were identified. Using mutation and recombination rates, they also hypothesized that the original sickle cell mutation arose 259 generations, or about 7,300 years, ago.
This period falls into the time range of the Holocene Wet Phase, a time in history characterized by a rainy and moist climate in northern Africa. Shriner and Rotimi suggested that the mutation could have originated in the Sahara region, back in the days when the Sahara resembled a savanna more than a desert. Alternatively, the mutation may also have come from the equatorial rainforests of west-central Africa.
Over time the mutation spread around Africa, perhaps carried by the Bantu people who expanded from modern day Nigeria across sub-Saharan Africa. It eventually reached the Arabian Peninsula, India and beyond, as suggested by the presence of the classical Arab-Indian haplotype in Kenyan and Ugandan subjects.
Many of those with two copies of the mutation likely died young. Those with only one copy, however, would have been better protected against the serious threat of malaria. They could still contract the disease but were less likely to develop and possibly die from the most severe manifestation, cerebral malaria. The advantage this conferred in regions where malaria is endemic ensured its continued existence.
It is still uncertain whether the patterns observed by Shriner and Rotimi exist across a larger number of carriers and individuals with sickle cell anemia, beyond the 156 involved in the recently published study.
This would be a further avenue of investigation, along with exploration of the newly defined haplotypes.
Researchers are hopeful that further investigation will shed light on differences in the severity of sickle cell anemia symptoms between individuals and provide more information toward an eventual cure.