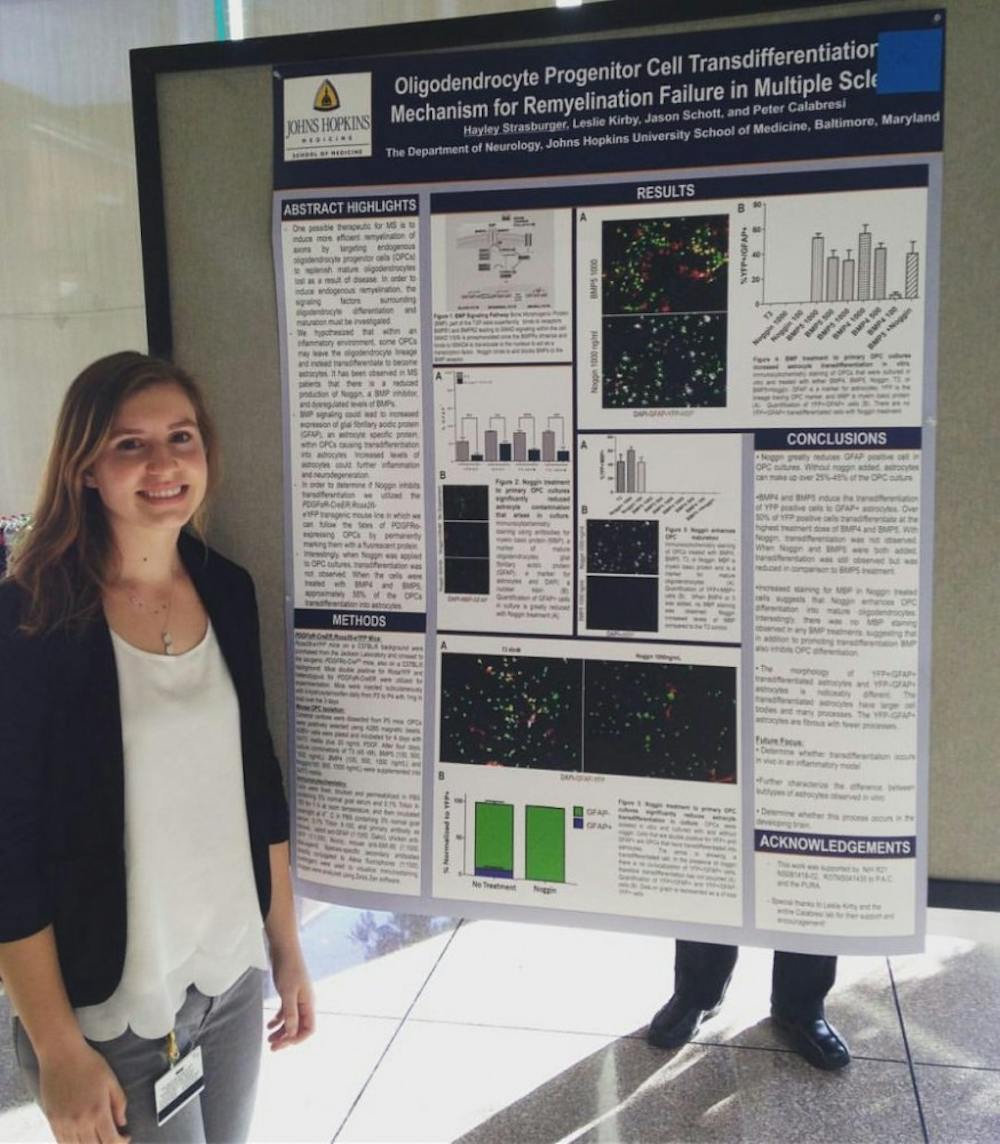
After barreling through a detailed explanation of her neuroscience research — throwing a “remyelination” here and an “endogenous oligodendrocyte” there — senior Hayley Strasburger casually mentions, “Oh, I came in as a history major.”
Strasburger is now a neuroscience major, and for the past three and a half years, she has intently studied multiple sclerosis (MS) in the Calabresi lab at the Johns Hopkins medical campus. She never would have started research (or even neuroscience in the first place) if it hadn’t been for Professor Stewart Hendry’s “Introduction to Neuroscience” course she took during her freshman fall.
After taking just a single class, neuroscience had her hooked. Eager to dive in, Strasburger began to look for research opportunities the following spring. Despite the breadth of neuroscience research available to her, she knew what she wanted to study: multiple sclerosis.
“My grandmother had MS, so I’d always known about it, but I didn’t really understand what it was until this neuroscience class,” Strasburger said.
So, Hendry guided her to the Calabresi lab, which explores how the immune system interacts with the central nervous system (the brain and spinal cord) in MS patients.
Through her work in the Calabresi lab, Strasburger began to expand her knowledge about MS and how it affects the nervous system. Everything happening right now in the human body — blinking, breathing and reading this article — is thanks to neurons. These cells link together to send signals throughout your body and are the core component of the central nervous system.
Each neuron has one axon, a long extension that branches off and connects with other nerve cells. The wire-like axon rapidly sends chemical and electrical signals, but not without the help of myelin, a fatty insulating material that forms a ‘sheath’ around the axon. In MS patients, the myelin coating is damaged, and the cells that make it, oligodendrocytes, are killed off by the patient’s own immune system.
Although no one knows the cause, the effect is well understood. Without myelin, your body’s signals are slowed or halted, resulting in the wide range of symptoms seen in MS patients: fatigue, dizziness, depression, speech problems, headaches, seizures, etc.
Patients with the most common form of MS called “relapsing-remitting MS” can regrow oligodendrocytes and repair some of the damage done between their MS attacks. Patients with the rarer form of the disease, progressive MS, experience slow, continual degradation of their myelin.
Despite this knowledge, there are treatments available only for relapse-remitting MS, but even those have numerous side effects like rashes, worsened depression and flu-like symptoms. There are no treatments for people who, like Strasburger’s grandmother, have progressive MS.
So the questions on many MS researchers’ minds are “What causes MS?” and “How can we help patients’ bodies repair myelin?” Strasburger’s work at the Calabresi lab focuses on the latter, looking at how the body naturally encourages more oligodendrocytes to grow and produce more myelin (in relapse-remitting patients) and how that process can be stimulated to happen faster in progressive MS patients.
“They center on how the immune system interacts with the central nervous system in MS patients, particularly seeing if they can encourage young oligodendrocytes to mature using what’s naturally in the brain,” Strasberger said.
To this end, Strasberger conceptualized, designed and carried out her own project in lab. She had noticed that in a petri dish of young oligodendrocytes, many would mature into astrocytes, another cell of the central nervous system.
A special type of protein, bone morphogenetic protein or BMP, stimulates this “transdifferentiation” process, and MS patients actually overproduce it.
Strasberger wanted to see if this excess BMP was forcing youthful oligodendrocytes to mature into astrocytes, which don’t produce the myelin MS patients lack. Strasberger points to the development of her very own project as one of her biggest successes.
“It was one of the coolest things, just having my own ownership of data and experiments,” she said.
However, it was also one of her biggest disappointments — she saw success in her petri dish studies, but couldn’t see the same effects in a mouse model.
Nevertheless, Strasberger is not discouraged and has already been accepted to a number of neuroscience Ph.D. programs for next year. She loves the freedom with academic research and enjoys that it’s hands on and different every single day.
“You always have to be thinking of new ideas,” she said.
At the same time, she also thoroughly recognizes that she have a very unique experience as Hopkins students.
“It’s such a great place for undergrads to be doing research. I’m meeting a lot of people from other schools at these [grad school] interviews that didn’t have this opportunity,” she said.
And while not everyone will fall in love with research as much as Strasberger has, she’s proven that you can step onto the Hopkins campus as a history major, have a true research experience and step off as a neuroscience Ph.D. candidate.