Tissue and organ failure that arises due to injury or other forms of damage is a major health issue and has motivated tremendous interest in the fields of tissue engineering and artificial organ research.
Collaboration across multiple fields, such as cell biology, polymer chemistry and regenerative medicine have created an artificial tissue prototype that revolutionizes fields such as transplantation medicine and drug delivery research, just to name a few.
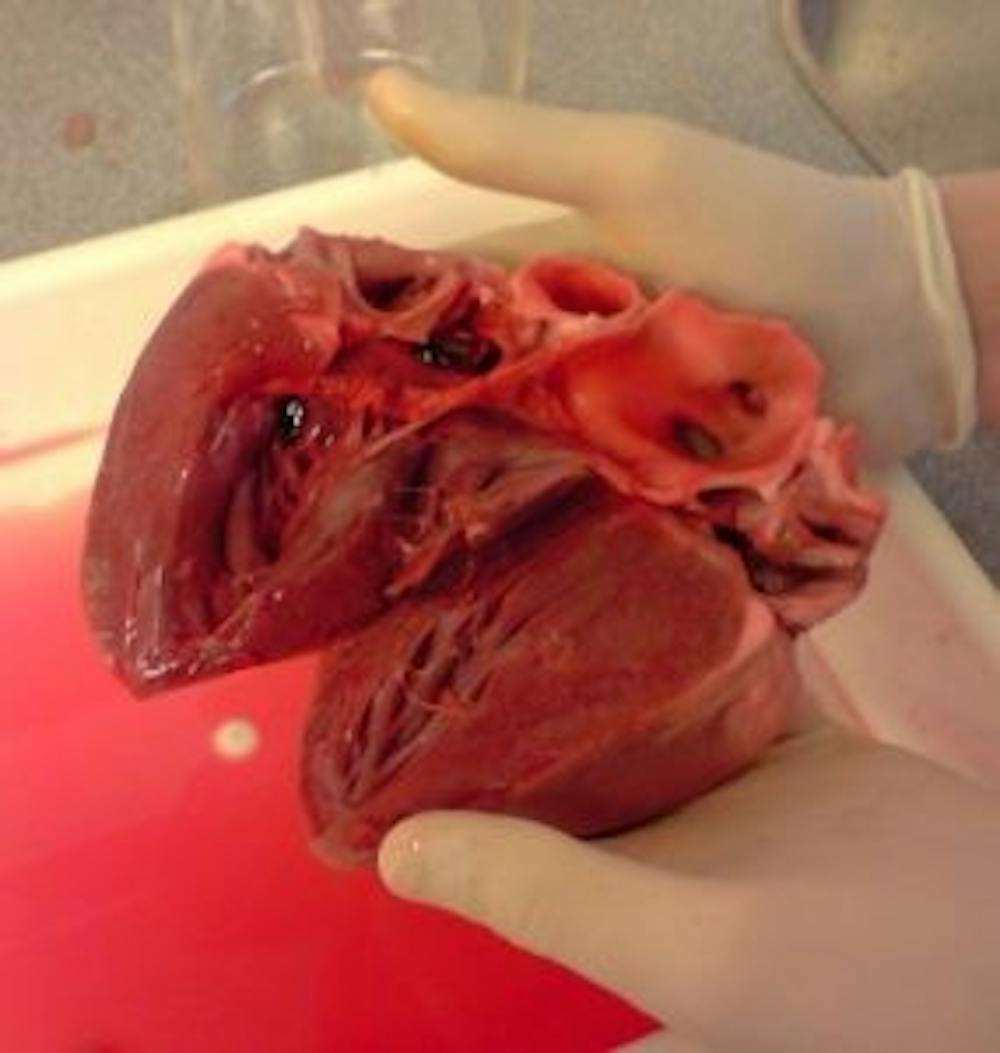
Actually generating 3-D functional cardiac tissue remains a challenge, however. The heart has a high cell density and comprises three different types of cells: contractile cardiac muscle cells, connective tissue cells and vascular cells.
“Making in vitro 3-D cardiac tissue has long presented a challenge to scientists because of the high density of cells and muscularity of the heart,” Dmitry Rogozhnikov, a Ph.D. student in chemistry at York University, said in a press release. “For 2-D or 3-D cardiac tissue to be functional it needs the same high cellular density and the cells must be in contact to facilitate synchronized beating.”
Current techniques used to assemble 3-D tissue involves polymer scaffolds by trapping cells. Although this method was a huge advancement, it poses several limitations.
One limitation is that scaffold reduces the formation of cell junctions, a critical part of intercellular communication in cardiac tissue. Cardiac tissues use cell junctions to send electrical signals to far away cells so that all cells beat in synchrony.
Professor Muhammad Yousaf of York University and his team of graduate students created the first scaffold-free 3-D cardiac tissue model that beats in harmony through the combination of liposome fusion, cell surface engineering and bio-orthogonal chemistry.
In their experiment, they harvested cardiac cells from newborn rats. Some of these fresh cardiac cells were then treated with a liposome reagent called ViaGlue. This ViaGlue strategy allows individual cardiac cells to click together rapidly to form stable, complex cardiac tissue.
Furthermore, Yousaf and his team tested two drugs known to affect heart rate, isoprenaline and doxorubicin, to both 2-D and 3-D cardiac tissues. Isoprenaline is a drug used to treat asthma and bradycardia (slow heart rate). Doxorubicin is a drug used to treat stomach cancer or leukemia.
Both tissues responded to the drugs in a similar fashion: increased heart rate when isoprenaline was applied and decreased heart rate when doxorubicin was applied. This result showed that the scaffold-free 3-D cardiac tissue can react according to drug stimulants.
Drugs that diffuse across 3-D cardiac tissue needs to pass multiple layers of cells, whereas in 2-D tissue only one layer must be passed. If a drug causes similar reactions to both 2-D and 3-D cardiac tissue, then the drug shows strong implications that it can reach its intended target in a real-life scenario.
Yousaf and his team believe that their results will have a significant impact on autocrine and paracrine signaling studies and evaluation of tissue for drug screening.
“This breakthrough will allow better and earlier drug testing and potentially eliminate harmful or toxic medications sooner,” Yousaf said.
In addition, Yousaf’s research could further impact treatments for cardiovascular diseases. According to the World Health Organization, cardiovascular diseases are the leading causes of death in the world and about 17.5 million people died worldwide from cardiovascular diseases in 2012.
Yousaf has created a start-up company called OrganoLinX to provide ViaGlue to the public and even custom 3-D tissues on demand.