By TONY WU Senior Staff Writer
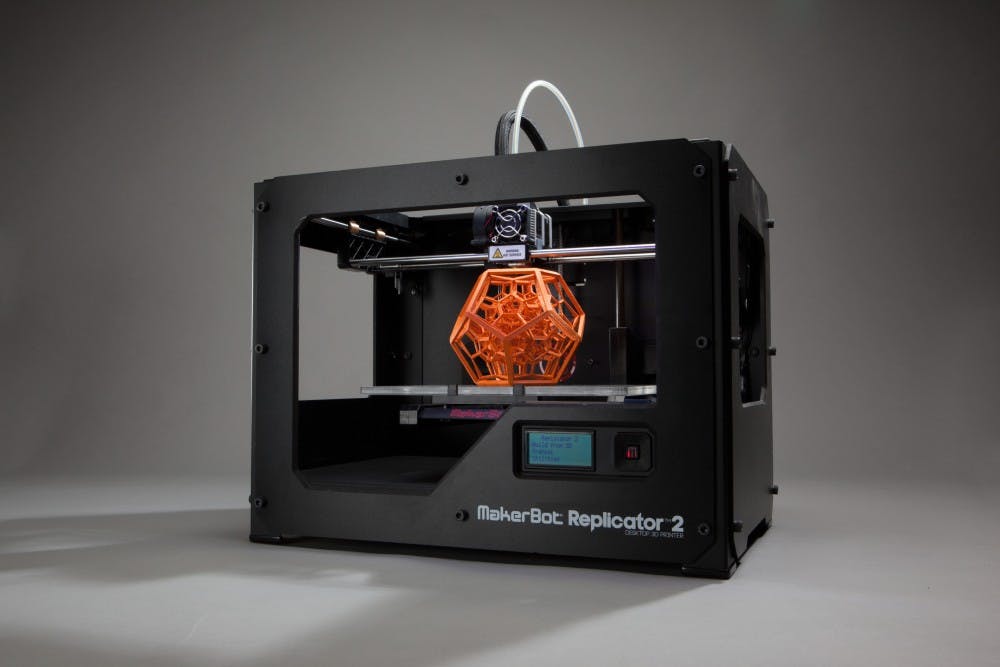
In recent years 3-D printers have captivated the public’s attention. With a template, a printer can produce a physical copy of almost anything in hours. To take advantage of this innovative manufacturing process, researchers at Carnegie Mellon University (CMU) have sought to use the concept of a printer to generate heart tissue.
Additive manufacturing, another name for 3-D printing, was first developed in the 1980s. Before the printing process begins, the printer undergoes fixup, which is a procedure that checks for errors in the design templates. After the file is verified, the program then slices the template into thin layers, allowing the printer to build the object layer-by-layer.
A group of scientists at CMU applied additive manufacturing to human hearts. First, they obtained MRI images of the arteries and 3-D images of hearts through CT scans. These images were then uploaded into the printer, which contains soft proteins and hydrogels. The hydrogel, a network of hydrophilic polymer chains, provides a scaffolding onto which cells can grow.
There are several challenges in tissue printing. First, the hydrogel is very soft and can deform under its own weight. Second, previous printing methods do not provide the necessary resolutions for complex microstructures in real tissues. There are also additional problems like keeping cells viable during the manufacturing process and the removal of any support materials used to build the tissue.
To address these issues, researchers developed a new printing method: FRESH. An acronym for freeform reversible embedding of suspended hydrogels, FRESH utilizes a support bath in the manufacturing of the tissue structures. The support bath consists of a second type of hydrogel that is thermos-reversible, meaning that it can be removed through heat.
The bath holds the shape of the tissue being printed, preventing the structure from collapsing under its own weight. The bath can then be removed from the printed structure by warming the printed tissue to 37 degrees Celsius, which is the temperature suitable for human cells.
The FRESH technique allowed scientists to create structures that resemble real tissues. An experiment sought to print a human vascular tree using various types of proteins and hydrogels. The MRI images are taken from the right coronary artery vasculature and uploaded into the printer. Though a consistent error was the increased thickness of the blood vessel walls compared to human tissues, the resulting structure was comparable to actual vasculature, with less than 15 percent variation in length and width.
Another experiment was conducted to compare FRESH printing and traditional printing techniques. An image of an embryonic chick heart was uploaded to the printer. Cross-sections of the resulting heart are obtained through multi-photon microscopes. While traditional techniques cannot replicate the complex structures, the FRESH prints resembled the 3-D model with less than 10 percent in variation.
Currently, more than 4,000 Americans are waiting for a heart transplant, putting pressure on the supply of human organs. To alleviate this, there is a growing focus on bioprinting, but most printers are expensive and require specialists to operate. The FRESH technique developed by the CMU researchers reduced the cost to less than $1,000 by using consumer-level printers and free software. These improvements to tissue printing techniques may reduce the strain by providing an alternative and cheap option in the future.