Indeed, scientists have developed a drug that promotes the growth of neural stem cells for the treatment of Parkinson’s. This drug is currently being tested in human clinical trials, holding much promise based on preliminary data and pre-clinical studies on animal models. If the drug is truly effective, it could be the first treatment ever able to slow or even halt the progression of neurodegenerative diseases.
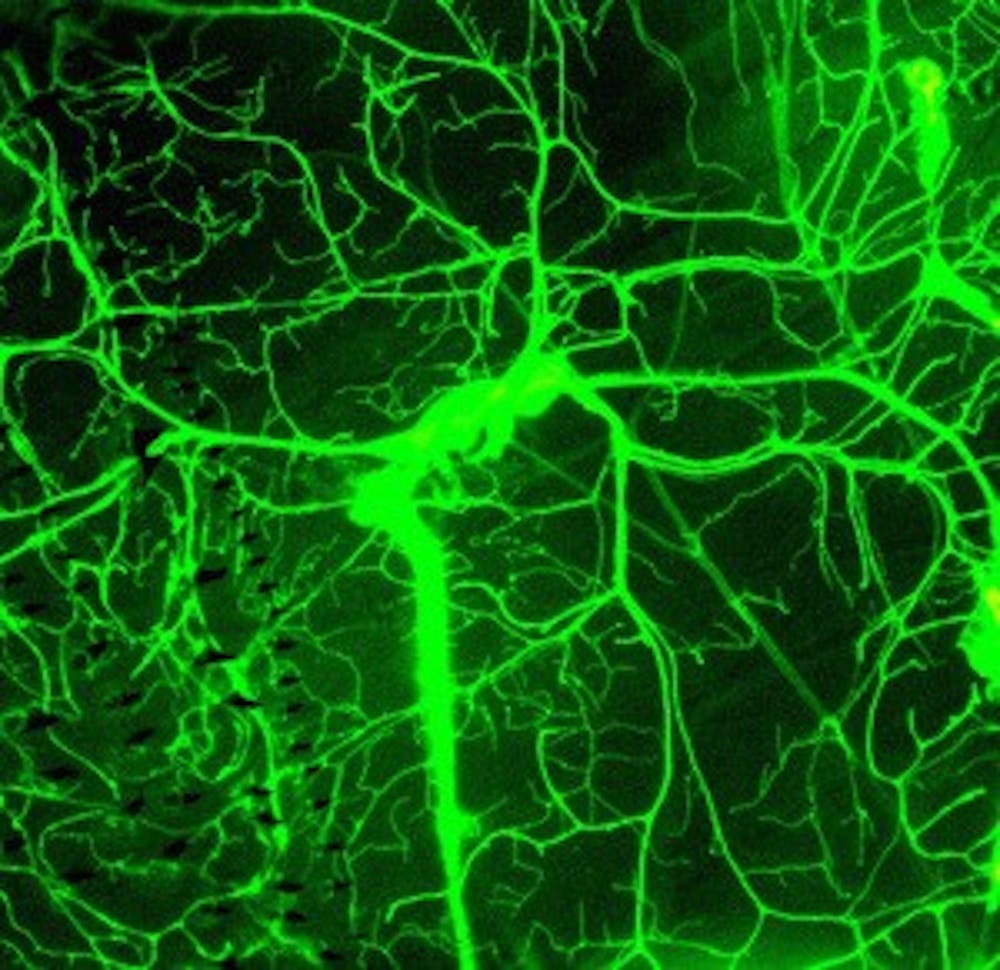
Although strategies to promote neurogenesis are exciting and promising, research into adult neural stem cells is still a relatively new field in comparison to the rest of neuroscience. The field of adult neurogenesis took off 20 years ago when Peter Eriksson and his colleagues showed that adult human brains are indeed capable of making new neurons. While much progress has been made since then regarding the biology of adult neural stem cells, many significant questions remain unanswered, ranging from the regulatory networks that control the brain’s stem cell niche to the contribution of adult neurogenesis to brain function.
Because there is still a lot to learn about these neural stem cells, we have to be cautious about adopting strategies to promote neurogenesis. As exciting as it may seem, simply increasing neurogenesis might not be the right answer for all conditions, and boosting neurogenesis might inadvertently cause adverse side effects.
The basis for boosting neurogenesis as a therapeutic avenue for the treatment of neurological disorders comes from the hypothesis that new neurons might either replace lost cells or provide support to surviving neurons. However, rather than having a regenerative effect, these new neurons might actually exacerbate the disease conditions. For example, instead of migrating to the injury sites, the new neurons may migrate somewhere else and disrupt healthy circuits. Indeed, in animal models of epilepsy, increased neurogenesis has been observed following recurrent seizures. It is believed that this excessive neurogenesis reorganizes the brain’s circuitry in such a way that makes it more prone to spontaneously initiating seizure activity and cognitive impairments in epilepsy.
In addition to the possibility of improper integration into healthy circuits, increasing neurogenesis might also exacerbate neuronal loss by depleting the population of neural stem cells. Let us consider neurodegenerative diseases as a condition that involves two opposing forces: neurodegeneration and regeneration. Thus, a neurodegenerative disorder, such as Alzheimer’s, involves a net loss of neurons because there is more degeneration than regeneration of neurons. In the short term it appears that increasing neurogenesis can overcome this net loss of neurons by stimulating regeneration. However, in the long term, constant regeneration will deplete the stem cell population. By then the brain will not have any more “fuel” to maintain regeneration, accelerating the progression of neuronal loss.
As promising as the stimulation of neurogenesis might sound, we also need to be cautious and carefully consider all of the possible implications that new neurons might have for the brain. Despite the desperate need for novel therapies, rushed research and clinical development can only lead to failures and disappointment in the long-term. In the end, as excited as I am about the field of adult neurogenesis, I need to emphasize that neural regenerative medicine represents a very small glimmer of hope that requires much more rigorous research and understanding before it can be reliably applied in the clinic.