The inner workings of tuberculosis — historically known as “consumption” and the “White Plague” — have remained shrouded in mystery since antiquity. However, tuberculosis’s estimated 5000-year reign of terror may soon be grinding to a halt. A recent study has discovered more about how our bodies react to bacteria that causes the disease.
The mechanisms for most types of bacterial infections and the body’s subsequent immune responses to the infection are well understood, but tuberculosis is an exception. Caused by the bacteria Mycobacterium tuberculosis, the disease is estimated to have infected approximately one-third of the world’s population at some point or another, with new infections occurring in one percent of the world’s population every year.
A recent study by researchers at the Hopkins School of Medicine has elucidated details about how a key molecule released by M. tuberculosis controls the ways in which the body combats tuberculosis infections. The researchers propose that adjusting the levels of this key molecule may be crucial to devising new vaccines and drugs to prevent and treat tuberculosis. William Bishai, co-director of the Hopkins Center for Tuberculosis Research Laboratory, led the study. A report of the study’s findings was published online in the medical journal Nature Medicine on Mar. 2.
When M. tuberculosis infects a host cell, it releases a molecule called cyclic di-adenosine monophosphate (c-di-AMP) into the host cell. C-di-AMP triggers type I interferon responses in the infected host cells. In general, type I interferons are produced when the body recognizes a virus has invaded it. This means that c-di-AMP produced by M. tuberculosis activates the same cellular defense mechanisms that viruses do.
Bishai suggests that M. tuberculosis is able to trick the human body into thinking it has encountered a virus rather than a bacteria, which may partially explain why human immune systems are often ineffective at combating tuberculosis infections.
In their first set of experiments, the researchers measured levels of bacterial c-di-AMP production in order to confirm that M. tuberculosis produces and secretes it. They found thatc-di-AMPlevels increase significantly when the bacteria are dividing and proliferating.
In the next set of experiments, the researchers asked whether c-di-AMP was responsible for altering host cell immune responses. They tested three different strains of the bacteria: one wild type unaltered strain and two genetically modified strains. In the first genetically altered strain, the bacteria overexpressed certain genes, known as di-adenylate cyclases. This strain produced approximately 20 times more c-di-AMP compared to the wild type strain. In the second strain, the bacteria’s di-adenylate cyclase genes were knocked out. The resulting strain produced no c-di-AMP.
Afterwards, the researchers infected three groups of mouse macrophage cells — white blood cells that play a key role in immunity — each with one of the three strains of M. tuberculosis. The researchers quantified and compared degrees of immune responses elicited by the different strains by measuring the levels of interferon-beta protein secreted by the macrophages.
Interferon-beta protein is a type I interferon protein primarily involved in immune responses against viral infections. The researchers found that increasing c-di-AMP release into the mouse macrophages corresponded with increasing interferon-beta protein secretion. In other words, higher levels of c-di-AMP resulted in stronger antiviral immune responses.
However, the researchers suggest that simply measuring interferon-beta levels cannot reveal a complete picture of what happens during a tuberculosis infection. In a third set of experiments, the researchers monitored the growth patterns of the three different M. tuberculosis strains inside the cells they’ve infected. The researchers found that the strain that overexpressed its di-adenylate cyclase genes and overproduced c-di-AMP demonstrated significantly slower growth rates when compared with the wild type strain. This indicates that overexpression of c-di-AMP by M. tuberculosis results in diminished bacterial growth.
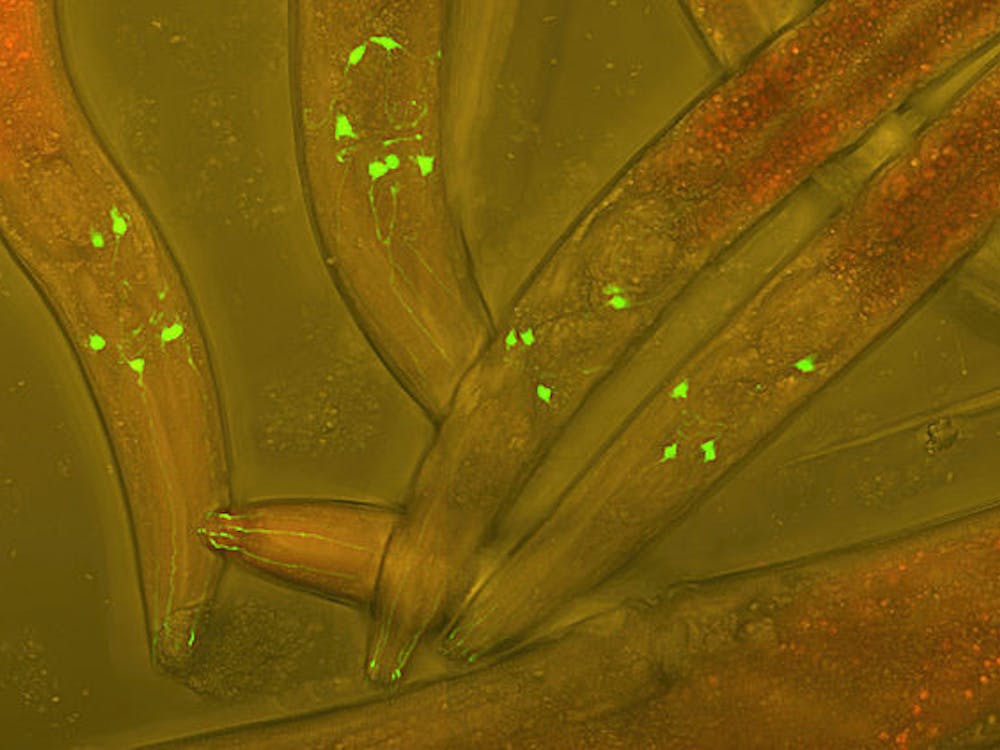
Previous studies have suggested that molecules similar to c-di-AMP can cause cells to degrade and dispose of its own cellular components in a process known as autophagy. The researchers also investigated whether or not excessive levels of c-di-AMP was triggering infected host cells to “eat” the tuberculosis bacteria. By labeling cells with fluorescent proteins and using microscopy, the researchers observed that cells infected with M. tuberculosis strains that overproduced c-di-AMP indeed underwent more autophagy than cells infected with M. tuberculosis strains producing lower amounts of c-di-AMP.
This observation led the researchers to question whether or not different levels of c-di-AMP could alter the severity of the tuberculosis disease. To test this, the researchers infected mice with the three different strains of M. tuberculosis. Mice infected with the strain that produced no c-di-AMP survived for only 77 days. Mice infected with the wild type strain survived for 150 days. Notably, mice infected with the strain that overproduced c-di-AMP survived for 321 days.
Bishai suggests that it is uncertain whether altering c-di-AMP levels could generate similar survival outcomes in humans or even whether different c-di-AMP levels could lead to different health outcomes in humans. Nevertheless, Bishai believes that the findings of the current study demonstrate that future human studies would be both meaningful and beneficial. The researchers suggest that future studies should focus on using the newly discovered knowledge about c-di-AMP to develop novel methods of preventing and treating tuberculosis as well as other related diseases.