Just as the severity of the Ebola epidemic has varied from country to country, the severity of the disease when contracted varies from person to person. Some people who contract the virus are able to completely resist the disease; some suffer varying severities of illness and eventually recover, while others succumb to internal bleeding, organ failure and death. A new study led by systems biologists and virologists Angela Rasmussen and Michael Katze at the University of Washington Department of Microbiology suggests that genetic factors may cause the wide range of responses to the Ebola virus.
Previous studies on people who had contracted the Ebola virus demonstrate that the person-to-person variation in disease severity is not attributed to specific changes in the Ebola virus itself that make it more or less harmless. Instead, it was an individual body’s attempts to fight off infection that seemed to determine disease severity.
Generally, in individuals who experienced severe or deadly disease, viral infection was detrimental to the activity of genes that promote blood vessel inflammation and cell death. In contrast, in individuals who survived the disease, viral infection spurred an increase in activity in genes that promote blood vessel repair and production of infection-fighting white blood cells.
Up to this point, animal studies on Ebola prevention and treatment have been limited by the lack of mouse models that replicate the key characteristics of human Ebola hemorrhagic fever. Instead, previous animal studies have been restricted to macaques, guinea pigs and Syrian hamsters, species whose usages are limited by practical and ethical concerns.
In this new study, Rasmussen, Katze and their research team developed a mouse model to examine the role that an individual’s genetic composition plays in the progression and prognosis of Ebola hemorrhagic fever. The research was conducted in a highly secure, state-of-the-art bio-containment safety level 4 laboratory at the National Institutes of Health Rocky Mountain Laboratories in Hamilton, Mont. The study was completed in full compliance with federal, state and local safety and biosecurity regulations. The specific virus used in the study has been used several times in previous research studies and was not altered in any way during the study.
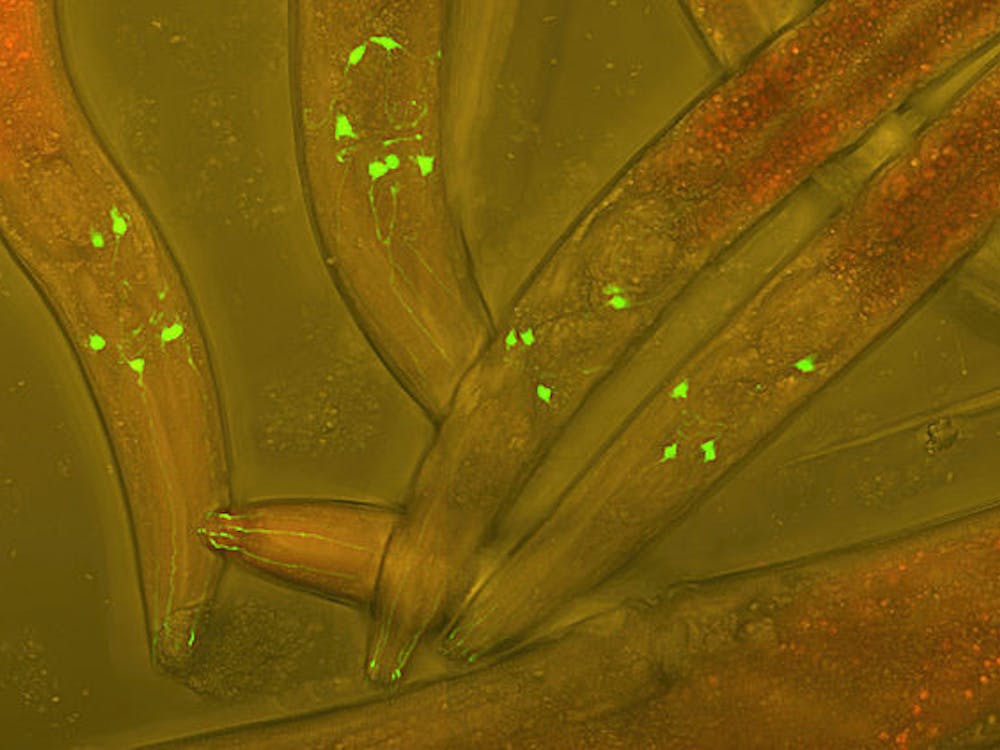
The researchers bred different strains of genetically diverse inbred laboratory mice and infected the mice with a mouse-adapted strain of the same species of Ebola virus causing the 2014 Ebola virus epidemic in West Africa. The researchers found that all of the mice lost weight within the first few days following infection. Afterwards, the mice began to exhibit an assortment of reactions toward the virus, which were classified into five categories.
Nineteen percent of the mice were categorized as “resistant.” These mice not only survived but also fully recovered and regained their lost weight within two weeks after infection. They showed no gross pathological evidence of the disease, and their livers looked completely normal. Eleven percent of the mice were categorized as “partially resistant.” Less than half of these mice died from the Ebola virus.
Seventeen percent of the mice were categorized as “lethal.” More than half of these mice died from the Ebola virus. Nineteen percent of the mice were categorized as “lethal with hepatitis.” In addition to having a mortality higher than 50 percent, these mice exhibited liver inflammation and discoloration but no classic symptoms of Ebola. Finally, 34 percent of the mice were categorized as “lethal with Ebola hemorrhagic fever.” In addition to having a mortality higher than 50 percent, these mice suffered from swollen spleens, internal bleeding, blood discoloration, changes in liver texture and color, and blood that took too long to clot. These characteristics are all hallmark symptoms of fatal Ebola hemorrhagic fever in humans as well.
Rasmussen suggests that the frequency of the various disease symptoms and outcomes observed across the different strains of mice in the study are similar both in characteristics and proportions to the spectrum of disease symptoms and outcomes observed in humans in the 2014 Ebola virus outbreak in West Africa. In other words, what was observed in the Ebola-infected mice in the study is a small-scale representation of what is happening among humans with Ebola in West Africa right now.
Katze believes that the study shows that genetic factors play a significant role in determining disease prognosis. It is also possible that recent Ebola survivors may have had immunity to either the Ebola virus or a related virus, which gave them a vital advantage during the epidemic.
The researchers hope that the findings of their study can be quickly applied to the development of clinical therapeutics and vaccines against the Ebola virus. The researchers believe that their mouse model can be used to pinpoint genetic markers, conduct detailed studies on the origin and progression of symptoms and assess drugs that have broad-spectrum anti-viral activities against all Zaire Ebola viruses, including (but not limited to) the one responsible for the current epidemic in West Africa.
The study was completed in collaboration with the National Institutes of Health Rocky Mountain Laboratories in Montana and with the University of North Carolina at Chapel Hill. The study was published in Science on Oct. 30.